The real difference between a yeast infection and bacterial vaginosis boils down to one simple thing: a yeast infection is a fungal overgrowth, while BV is a bacterial imbalance. Getting this right is absolutely critical because they need completely different treatments. An accurate diagnosis is your first step toward getting relief.
Understanding the Key Differences
Trying to figure out what’s going on down there can be confusing, especially since both yeast infections and BV can cause irritation and weird discharge. But there are a few tell-tale signs that can point you in the right direction before you get a final answer from a doctor.
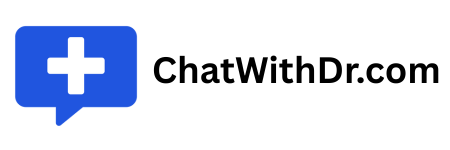
A yeast infection, which is caused by an overgrowth of the fungus Candida, is notorious for its intense, maddening itch and a thick, white discharge. On the other hand, bacterial vaginosis happens when the natural balance of your vaginal microbiome gets thrown off, allowing certain bacteria to take over. This imbalance typically leads to a thin, grayish discharge and a very distinct, fishy odor.
This chart breaks down the biggest complaints for each condition—the itch of a yeast infection versus the odor of BV.
While both are uncomfortable, what bothers you most is often the biggest clue you have for an initial self-assessment.
To help you sort through the symptoms, here’s a quick side-by-side comparison of what you’ll typically see with each condition.
Key Differences: Yeast Infection vs. BV
| Symptom/Characteristic | Yeast Infection (Candidiasis) | Bacterial Vaginosis (BV) |
|---|---|---|
| Primary Cause | Fungal overgrowth (Candida) | Bacterial imbalance (overgrowth of anaerobic bacteria) |
| Discharge Color & Texture | Thick, white, clumpy (like cottage cheese) | Thin, watery, grayish-white or yellow |
| Odor | Usually minimal or slightly yeasty (like bread) | Strong, unpleasant fishy smell, especially after sex |
| Primary Sensation | Intense itching, burning, and irritation | Mild irritation or itching; sometimes no symptoms at all |
| Vaginal pH | Normal (below 4.5) | Elevated (above 4.5) |
| Common Triggers | Antibiotic use, hormonal changes, weakened immunity | Douching, new or multiple sexual partners |
This table makes it clear that while some symptoms overlap, the underlying causes and key characteristics are worlds apart.
Why Getting it Right Matters
Guessing wrong means you’ll use the wrong treatment, which only prolongs your discomfort. For example, grabbing an over-the-counter antifungal cream for BV won’t touch the bacterial imbalance and just delays the proper care you actually need.
The most common mistake I see is patients self-treating a presumed yeast infection when it's really bacterial vaginosis. Since BV needs prescription antibiotics and a yeast infection needs antifungals, getting the right diagnosis the first time is everything for fast, effective relief.
Knowing these core differences is a great start. While this guide is helpful, only a healthcare professional can give you a definitive diagnosis—especially if this is your first time with these symptoms, you’re pregnant, or the infections keep coming back. A proper diagnosis is the only way to get the targeted treatment you need to restore your vaginal health.
Understanding What Disrupts Your Vaginal Balance
Think of your vaginal environment as a finely tuned ecosystem. It’s naturally dominated by helpful bacteria, mostly a type called Lactobacillus, which produces lactic acid to keep things healthy and acidic. This acidity is a fantastic natural defense, preventing less friendly bacteria and fungi from getting out of hand.
But like any ecosystem, this delicate balance can be thrown off. When that happens, either a fungus like Candida or certain bacteria can multiply way too fast, leading to an infection and all the uncomfortable symptoms that come with it. The specific trigger is often what decides which condition you end up with.

What Causes a Yeast Infection
A vaginal yeast infection, also known as vulvovaginal candidiasis, is a fungal infection. It's almost always caused by an overgrowth of Candida albicans, a type of yeast that normally lives in the vagina in small, harmless numbers.
When something disrupts the vaginal environment, Candida seizes the opportunity to multiply like crazy.
Common triggers that give yeast an opening include:
- Antibiotic Use: Broad-spectrum antibiotics are great at killing the bad bacteria causing your sinus infection, but they also wipe out the good Lactobacillus bacteria. This gives yeast a clear path to flourish.
- Hormonal Shifts: Any big swing in estrogen—from pregnancy, birth control pills, or hormone therapy—can change the vaginal environment and make it a more inviting place for yeast to grow.
- Weakened Immune System: Conditions like unmanaged diabetes or taking medications that suppress the immune system make it harder for your body to keep Candida levels in check.
It's also helpful to have a broader picture of how different things, like understanding hormonal factors, can affect your body's overall balance.
What Causes Bacterial Vaginosis
Bacterial vaginosis (BV) is completely different—it's not a fungal issue but a bacterial one. It happens when the population of good Lactobacillus bacteria drops, allowing other bacteria, especially anaerobic types like Gardnerella vaginalis, to take over.
This microbial shift makes the vaginal pH less acidic, creating the perfect conditions for these other bacteria to thrive.
A key point to remember is that BV is an imbalance of bacteria already present in the vagina; it is not a sexually transmitted infection (STI), though certain sexual activities can increase your risk.
Common risk factors linked to BV are:
- Douching: This practice is a major culprit. It washes away the protective Lactobacillus and disrupts the natural pH, leaving you vulnerable to bacterial overgrowth.
- New or Multiple Sexual Partners: While BV isn't an STI, sexual activity can introduce new bacteria or simply alter the vaginal ecosystem, raising the risk.
- Using Scented Products: Scented soaps, bubble baths, and feminine sprays can easily irritate sensitive vaginal tissues and throw the microbial balance off-kilter.
While both conditions are incredibly common, their incidence rates follow clear patterns. BV tends to be slightly more common than yeast infections, with both peaking in women of reproductive age. The highest incidence for yeast infections is in the 20–29 age group, while BV rates are most prevalent among sexually active women. The first step toward prevention is figuring out your own potential triggers.
Comparing Symptoms: A Definitive Breakdown
When you’re dealing with discomfort down there, trying to figure out if it’s a yeast infection or bacterial vaginosis can feel like a frustrating guessing game. While both can cause irritation, their key symptoms are usually distinct enough to give you some pretty strong clues. Pinpointing these differences is your first step toward getting the right help.
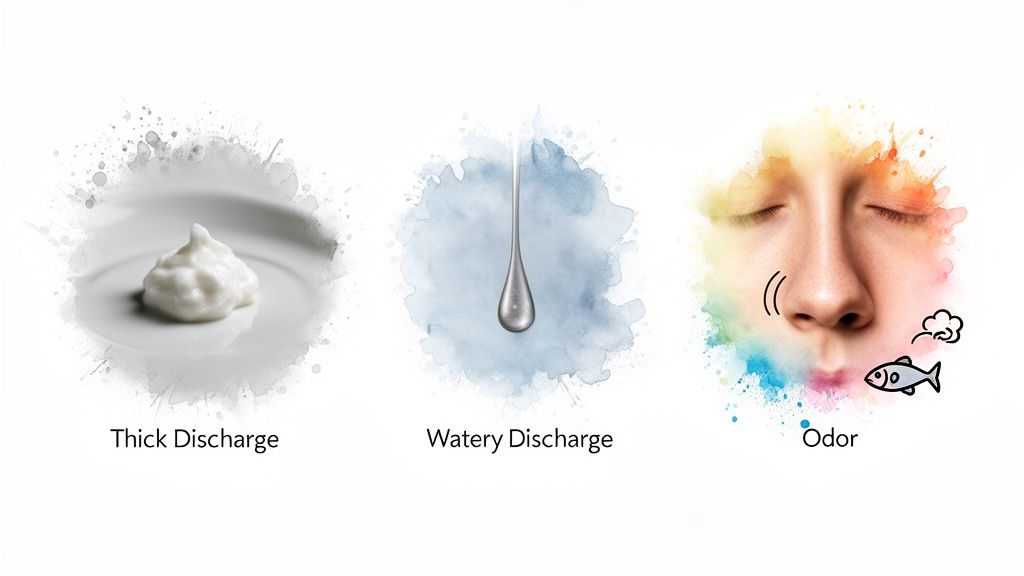
The three most telling signs are the discharge, any associated odor, and the specific sensation you feel. Each of these shows up differently depending on whether the cause is fungal or bacterial. Paying close attention to the details is the best way to understand what your body is trying to tell you.
Discharge Consistency and Color
The most visible difference between a yeast infection and BV is almost always the discharge. Think of it as the primary indicator, since the characteristics are practically opposites.
A classic sign of a yeast infection is a thick, white, and clumpy discharge. It’s often described as looking like cottage cheese and is typically odorless or has a very mild, bread-like scent. This unique consistency is a direct result of an overgrowth of the fungus Candida.
On the other hand, bacterial vaginosis produces a discharge that is thin, watery, and usually a grayish-white or even yellowish color. It tends to be more noticeable in volume and often coats the vaginal walls. This change comes from an imbalance in your vaginal bacteria, not a fungus.
Odor: The Unmistakable Clue
Odor is probably the single most revealing symptom when comparing a yeast infection vs. BV. The presence—or absence—of a distinct smell can almost immediately point you in the right direction.
Bacterial vaginosis is almost always associated with a strong, unpleasant fishy odor. This smell often gets more noticeable after sex or during your period, since semen and blood can alter the vaginal pH and make the scent stronger.
Yeast infections, in contrast, are typically odorless. If you notice any smell at all, it’s usually faint and yeasty, kind of like bread or beer. The lack of a foul odor is a huge sign that you’re likely dealing with a fungal issue rather than a bacterial one.
Sensation: Itching vs. Irritation
How it feels is another crucial piece of the puzzle. The type and intensity of discomfort you’re experiencing can vary a lot between the two conditions.
Here’s a head-to-head comparison of the primary sensations:
- Yeast Infection Sensation: The hallmark of a yeast infection is intense itching and burning. This can affect both the vagina and the vulva, often becoming severe and leading to redness, swelling, and significant discomfort. Pain during urination or sex is also common because the tissues are so inflamed.
- BV Sensation: Bacterial vaginosis usually causes only mild irritation or itching, if any at all. In fact, up to 50% of people with BV report no symptoms besides the tell-tale discharge and odor. The main complaint is rarely intense itching; it’s almost always about the discharge and smell.
This table breaks down the symptomatic differences side-by-side for a clearer view.
| Symptom | Yeast Infection (Candidiasis) | Bacterial Vaginosis (BV) |
|---|---|---|
| Discharge | Thick, white, cottage cheese-like | Thin, watery, grayish-white |
| Odor | Odorless or faintly yeasty | Strong, fishy smell |
| Main Sensation | Intense itching and burning | Mild irritation or none at all |
| Associated Pain | Common, especially during sex or urination | Uncommon |
While understanding these nuances is key, self-diagnosis can still be tricky. Symptoms can overlap, and other conditions like trichomoniasis can mimic these signs. Sometimes, symptoms like painful urination might even point to urinary tract issues. If you’re experiencing that alongside other symptoms, it’s helpful to know how to get fast online UTI treatment to rule out other causes. For a truly accurate diagnosis and the right treatment plan, a professional medical opinion is always your safest and most effective bet.
How Doctors Tell the Difference for Sure
Trying to figure out whether it's a yeast infection or BV based on symptoms alone is a tough—and risky—game. The overlap can be confusing, and honestly, other conditions can feel pretty similar. To get the right treatment, you absolutely need a real diagnosis from a clinician. They use a few simple, quick tests to get a clear picture of what’s going on.
The process usually kicks off with a chat about your symptoms and health history, followed by a pelvic exam. During the exam, your doctor will look for visible signs of irritation and take a small sample of vaginal discharge with a cotton swab. That little sample is the key to everything, allowing for some immediate in-office testing.
The Key Diagnostic Tests
Once that sample is collected, your doctor can run a few fast tests to nail down the cause of your symptoms. These methods are designed to pinpoint exactly which microbes are out of balance.
- Vaginal pH Test: This is almost always the first step. A small strip of pH paper is touched to the vaginal wall or the discharge sample. A healthy vaginal pH is acidic, typically below 4.5. A yeast infection usually doesn't change this, but BV makes the environment more alkaline, pushing the pH above 4.5. This test alone provides a huge clue.
- The "Whiff Test": It might sound a little strange, but this test is incredibly good at identifying BV. A drop of potassium hydroxide (KOH) is added to the discharge sample. If a strong, fishy odor is suddenly released, that's a classic sign of bacterial vaginosis.
- Microscopy: This is the gold standard. Your clinician will place a tiny bit of the sample on a glass slide and look at it under a microscope. This direct look lets them see exactly what’s causing the trouble.
Under the microscope, a clinician can clearly see the budding yeast cells and hyphae that scream "yeast infection," or they can spot the "clue cells" that confirm bacterial vaginosis. Clue cells are vaginal epithelial cells totally covered in bacteria, giving them a distinct stippled look—a dead giveaway for BV.
These tests are so important because, believe it or not, you can have both infections at once. Multiple studies confirm that BV and yeast infections are the top reasons for vaginal complaints, with BV being the most common culprit. A World Health Organization analysis estimated that 23–29% of women of reproductive age worldwide have BV. Some studies have even found that a coinfection with both BV and yeast happens in about 5% of symptomatic women, which is exactly why professional testing is a must.
Why an Accurate Diagnosis Is Non-Negotiable
Getting it right from the start means you get the right medication—antifungals for yeast, antibiotics for BV. Using the wrong treatment won't just fail to help; it can actually make the infection worse or lead to it coming back again and again.
Plus, a proper exam can rule out other potential causes, like sexually transmitted infections (STIs). If you have any concerns about other possibilities, you can explore options for confidential online STD testing to get total peace of mind. A real diagnosis is the only way to get fast, effective relief and protect your long-term reproductive health.
Navigating the Right Treatment Options
Figuring out if you have a yeast infection or bacterial vaginosis is more than just a medical curiosity—it’s the key to getting the right treatment. One is a fungal overgrowth, and the other is a bacterial imbalance, which means their treatments aren’t interchangeable. Using the wrong medication won’t just leave you feeling miserable; it can prolong your discomfort and even make the underlying problem worse.
The absolute first step is a confirmed diagnosis. It's a common mistake to self-diagnose and grab the wrong product from the pharmacy, which only delays getting proper care. For example, if you use an antifungal cream for BV, it will do absolutely nothing to fix the bacterial imbalance, letting the infection continue unchecked.

Treatment for Yeast Infections
Yeast infections are handled with antifungal medications, which are specifically designed to knock out the overgrowth of Candida fungus. You’ve got a few options here, from over-the-counter remedies to more powerful prescription solutions.
Over-the-Counter (OTC) Options:
If you’ve had a yeast infection before and recognize the tell-tale signs, OTC products are a go-to first step. These usually come in a few forms:
- Antifungal creams or ointments (like miconazole or clotrimazole) that you apply directly to the irritated area.
- Vaginal suppositories, which are inserted into the vagina, usually at bedtime for one or more nights.
Prescription Medications:
When OTC treatments don’t cut it, or if you’re dealing with a severe or recurring infection, a doctor will likely prescribe something stronger. The most common prescription is fluconazole, an oral antifungal pill that’s often effective with just a single dose. For more stubborn cases, your doctor might recommend a longer course of treatment.
A crucial piece of advice for anyone considering treatment: If this is your first time with these symptoms, or if you're even a little unsure what's going on, it's always best to see a clinician. A correct diagnosis is everything.
Treatment for Bacterial Vaginosis
Bacterial vaginosis requires a totally different game plan. Because it’s a bacterial issue, BV has to be treated with prescription antibiotics. There are no effective over-the-counter treatments for BV, which makes a doctor's visit essential.
Common antibiotics prescribed for BV include:
- Metronidazole: This can be taken as an oral pill or used as a topical gel inserted into the vagina.
- Clindamycin: This is often prescribed as a cream or ovule for vaginal application.
- Tinidazole: Another oral antibiotic option, which is sometimes used if metronidazole isn't working.
It is absolutely critical to finish the entire course of antibiotics your doctor prescribes, even if you start feeling better right away. Stopping early can lead to a quick recurrence of the infection because not all the disruptive bacteria have been eliminated. This is how people get stuck in a frustrating cycle of recurring BV.
When to Choose OTC vs. Prescription
Trying to decide whether to grab a product at the drugstore or get medical advice can be confusing. Here’s a simple guide to help you make the right call in the yeast infection vs bv dilemma.
Consider an OTC Yeast Infection Treatment If:
- You have been diagnosed with a yeast infection by a doctor in the past.
- You are 100% certain your current symptoms (thick, white discharge; intense itching; no foul odor) match your previous yeast infection.
- You are not pregnant.
You Must See a Doctor For a Prescription If:
- You suspect you have bacterial vaginosis (thin, grayish discharge with a fishy odor).
- This is your first time experiencing these types of symptoms.
- Your symptoms are severe, or OTC treatments haven’t provided any relief.
- You are pregnant or have a weakened immune system.
Dealing with healthcare can feel like a hassle, but modern options make it much easier. For those who need a clear diagnosis and fast access to treatment, you can get an online prescription from a board-certified doctor, often on the same day. This ensures you get on the correct treatment path without delay.
Preventing Recurrence and Understanding Risks
Dealing with a vaginal infection is frustrating enough the first time around. When it keeps coming back, it can feel like a never-ending cycle of discomfort. Understanding what triggers these recurrences and the risks of leaving them untreated is the first step to breaking that cycle for good.
For both yeast infections and bacterial vaginosis, prevention really comes down to protecting the delicate microbial balance in your vagina. A few simple, consistent habits can make a huge difference in keeping disruptive bacteria and fungi in check.
Proactive Steps for Vaginal Health
Small adjustments to your daily routine can create an environment where healthy bacteria thrive, seriously cutting down the chances of an imbalance. The goal is to avoid disrupting the natural acidity and protective flora that keep your vaginal ecosystem healthy.
Here are some practical prevention tips:
- Wear Breathable Underwear: Stick with cotton underwear instead of synthetic fabrics. Cotton lets air circulate, which helps keep the area dry and makes it a less welcoming place for yeast and bacteria to overgrow.
- Avoid Douching: Douching washes away the beneficial Lactobacillus bacteria that are essential for maintaining a healthy vaginal pH. Your vagina is self-cleaning, and douching only messes with this natural process.
- Use Gentle Hygiene Products: Use mild, unscented soaps and warm water for external cleansing only. Scented soaps, bubble baths, and feminine sprays can cause irritation and throw your pH balance completely off kilter.
A healthy vaginal environment is your body's best defense. The less you interfere with its natural balance, the better it can protect itself from the imbalances that lead to both yeast infections and BV.
The Risks of Recurrent and Untreated Infections
While both conditions are common, they aren't something to ignore, especially if they keep coming back. Chronic infections can signal underlying issues, and untreated BV, in particular, carries some significant health risks.
Recurrent vulvovaginal candidiasis (RVVC), which is defined as three or more yeast infections a year, affects up to 5–8% of women. While 75% of women will have at least one yeast infection in their lifetime, nearly 50% may experience a recurrence. Untreated bacterial vaginosis poses more severe risks, as it's linked to an increased likelihood of acquiring HIV and other STIs. It can also lead to serious pregnancy complications like preterm birth if left untreated.
For those interested in complementary approaches, some research explores things like the antifungal properties of aloe vera.
Why Consistent Medical Guidance Matters
If you feel like you're stuck in a cycle of recurrence, self-treating isn't the answer. A clinician can help you figure out the root cause, which could be anything from unmanaged diabetes to a resistant strain of yeast. They can prescribe a long-term management plan, like a scheduled course of antifungal medication for RVVC or targeted antibiotics for chronic BV.
Breaking the cycle for good requires a proper diagnosis and a consistent, medically guided strategy. This proactive approach not only brings relief but also protects you from the more serious health complications tied to untreated infections.
When You Should See a Doctor
Let's be honest, trying to self-diagnose a vaginal infection is a risky game. It’s tempting to grab an over-the-counter remedy and hope for the best, but the symptoms of a yeast infection versus BV can be incredibly misleading. Getting it wrong only drags out your discomfort and can sometimes lead to bigger problems down the road.
Knowing when to stop guessing and talk to a professional is the key to getting fast, effective relief. If you treat what you think is a yeast infection and see zero improvement—or things get worse—that's a huge red flag. It’s a clear sign the treatment isn’t working because the diagnosis is probably wrong.
Key Scenarios Requiring Medical Advice
Navigating symptoms on your own is confusing, but there are definite signals that it’s time to seek medical care. Don't hesitate to reach out to a doctor if you find yourself in any of these common situations.
Here are the specific times when seeing a doctor is non-negotiable:
- It’s Your First Time: If you’ve never had these symptoms before, you have no baseline to compare them to. A doctor needs to confirm the diagnosis and rule out other conditions.
- You're Unsure of the Diagnosis: Do your symptoms not fit neatly into one box? For example, if you have the classic itching of a yeast infection but also a fishy odor, it's essential to get clarity.
- Over-the-Counter Treatments Have Failed: You've finished a full course of an OTC antifungal and you're not feeling better. This could mean you have BV or even a resistant strain of yeast that needs prescription-strength medication.
- You Are Pregnant: Any vaginal infection during pregnancy must be managed by a clinician to ensure both your safety and the baby’s.
- Your Symptoms Are Severe or Recurrent: We're talking intense pain, swelling, or infections that keep coming back (three or more times a year). This signals a need for a much more robust treatment plan.
Seeking a professional diagnosis isn't just about getting the right medication. It's about making sure you don't have a more serious underlying issue, like an STI or a different skin condition, that requires a completely different approach.
The Modern Solution: Telemedicine
Thankfully, getting a professional medical opinion no longer means trying to schedule an in-person visit weeks from now. Modern telemedicine has completely changed the game, offering a convenient and highly effective way to get the care you need right from home.
This approach connects you with a board-certified physician who can review your symptoms through a secure, private intake process. Based on your information, they can provide an accurate diagnosis and, if needed, send a prescription straight to your local pharmacy.
It’s a fast, discreet, and reliable alternative for getting the correct care without the hassle of a traditional office visit. In many cases, you can have a diagnosis and a treatment plan in just a few hours.
Stop guessing and get a clear answer today. ChatWithDr offers same-day, text-based consultations with board-certified U.S. doctors for just $39.99. Get a diagnosis and prescription sent to your pharmacy, often within hours. Start your confidential consultation now.