For many women, a yeast infection starts with a familiar, unwelcome feeling: an intense itch that just won’t quit. The classic signs usually include that persistent vaginal and vulvar itching, a burning sensation, and a thick, white discharge often compared to cottage cheese. The good news? It’s typically odorless. These symptoms can be a minor nuisance or completely throw off your day-to-day life.
Recognizing the Telltale Signs of a Yeast Infection

Understanding what a yeast infection feels and looks like is the first step to getting relief—and fast. While most women share a core set of symptoms, how intense they are can vary from person to person. Think of your body as a finely tuned ecosystem; when the balance is off, it sends out clear signals.
The most prominent and frustrating symptom for most is that relentless itch. This isn't a fleeting irritation but a constant one, affecting both the vagina and the vulva (the outer tissues). This often comes with soreness, redness, and swelling, making the whole area feel raw and sensitive.
The Most Common Symptoms Explained
Beyond the itch, there are a few other key clues that point toward a yeast infection. Paying close attention to these changes can help you tell the difference between a yeast infection and other issues, so you can find the right care.
These common signals include:
- Vaginal and Vulvar Itching: An intense, distracting itch is the hallmark symptom for most women.
- Burning and Discomfort: This often feels like a stinging or raw sensation, which can get worse during urination or sex.
- Redness and Swelling: The vulva might look inflamed, red, and swollen from all the irritation.
- Thick, White Discharge: The classic visual sign is a thick, lumpy, white discharge that’s odorless.
- Vaginal Rash: Some women might also notice a rash or small, pimple-like bumps on the vulva.
This cluster of symptoms is more than just a physical hassle; it can be a major source of stress that disrupts your life. It’s a harsh reality for about 138 million women worldwide each year who deal with recurrent vulvovaginal candidiasis (RVVC), a severe and recurring form of yeast infection. You can get more insights on this global health issue and its impact from the landmark study.
A Quick Guide to Symptom Identification
To help you sort through what you’re feeling, the table below breaks down the key symptoms. It’s a simple way to cross-reference your experience and understand what to look for when your body feels out of balance.
Common Yeast Infection Symptoms at a Glance
| Symptom | What It Feels and Looks Like | Common Misconceptions |
|---|---|---|
| Itching | A persistent, often intense itch in and around the vagina. | Mild itching isn't always a yeast infection; it can also be caused by irritants like soap or fabric. |
| Discharge | Thick, clumpy, white, and odorless—similar to cottage cheese. | Not all discharge is a sign of infection. A fishy odor is more indicative of bacterial vaginosis (BV). |
| Burning | A stinging or raw feeling, especially when urinating or during sex. | This is often mistaken for a urinary tract infection (UTI), but UTIs typically involve frequent urination. |
| Redness & Swelling | The vulva appears visibly red, inflamed, and swollen. | Redness can also result from an allergic reaction or chafing, but with a yeast infection, it's paired with other key symptoms. |
This at-a-glance guide should make it easier to pinpoint what’s going on. Recognizing these signs quickly is your best bet for getting effective treatment and feeling like yourself again.
What Causes Your Body's Balance to Shift
Think of your vaginal microbiome as a carefully tended garden. In this garden, helpful bacteria like Lactobacillus are the diligent gardeners, working hard to maintain a slightly acidic environment. This acidity keeps the weeds—in this case, a fungus called Candida—from taking over. A tiny bit of this yeast is totally normal, but a yeast infection happens when this beautiful balance gets thrown off, allowing the Candida to grow out of control.
This disruption isn’t just random. It’s almost always triggered by specific factors that change the "soil" of your internal garden. Figuring out these triggers is the first step to understanding why you’re dealing with symptoms and how you can stop them from coming back.
The Impact of Antibiotics
One of the most frequent culprits behind a yeast infection is a course of antibiotics. While these drugs are lifesavers for fighting off nasty bacterial infections like strep throat or a UTI, they have a major downside: they can't tell the difference between bad bacteria and the good guys protecting your vagina.
Antibiotics are basically a broad-spectrum weed killer that, unfortunately, wipes out your helpful garden plants, too. Without the protective Lactobacillus to keep the yeast in line, Candida gets the perfect chance to multiply and cause those all-too-familiar, frustrating symptoms.
Hormonal Fluctuations and Their Effects
Hormones, especially estrogen, are major players in keeping your vaginal environment stable. When estrogen levels swing up or down, the delicate balance of your microbiome can shift with them, creating the perfect conditions for yeast to flourish.
This is why yeast infections often pop up during certain life stages or when you’re taking specific medications:
- Pregnancy: The surge in estrogen during pregnancy can change your vaginal pH, making it a more welcoming place for yeast.
- Birth Control: Hormonal contraceptives that raise estrogen levels can have the same disruptive effect on your natural balance.
- Menstrual Cycle: Many women find they’re more susceptible to infections right before their period, all thanks to those cyclical hormonal changes.
These hormonal shifts essentially change the composition of your garden’s soil, sometimes making it far more favorable for yeast than for your protective bacteria.
Understanding the root cause is crucial for effective management. For example, recognizing the signs of various yeast infections, such as when you identify what causes nipple thrush, can help in early detection and treatment, especially for new mothers who may be breastfeeding.
Underlying Health Conditions and Lifestyle Factors
Your overall health is the foundation for your body's entire ecosystem. Certain health conditions and even day-to-day habits can weaken your defenses, making it much easier for a yeast overgrowth to happen and for yeast infection symptoms in women to appear.
Uncontrolled diabetes is a huge risk factor. When your blood sugar is high, there’s more sugar in all your bodily fluids, including vaginal secretions. This excess sugar acts like a super-fertilizer for yeast, feeding its growth and leading to infections that are frequent or hard to shake.
Likewise, a weakened immune system can't do its job of managing the Candida population. Conditions that compromise immunity, like HIV, or treatments such as chemotherapy, leave your body vulnerable to all sorts of opportunistic infections—yeast overgrowth included. Even things like high stress or not getting enough sleep can temporarily dampen your immune response, giving yeast an opening. By understanding what throws your body off balance, you can take smarter, more proactive steps toward prevention and finally get some lasting relief.
Is It a Yeast Infection or Something Else Entirely?
When you’re dealing with frustrating vaginal symptoms, it's easy to jump to conclusions. You feel that all-too-familiar itch and see a change in discharge, and your first thought is almost always a yeast infection. But the world of vaginal health is more complex than that, and several other conditions can show up with strikingly similar signs.
Trying to self-diagnose can feel like navigating a maze without a map. Getting it wrong doesn't just mean waiting longer for relief—it could mean using the wrong treatment entirely, which might make the real problem even worse. The key is to understand the subtle but crucial differences between the most common culprits.
Unpacking the Symptom Overlap
The main sources of confusion are usually Bacterial Vaginosis (BV) and a common Sexually Transmitted Infection (STI) called trichomoniasis. Both share symptoms with yeast infections, like itching and changes in discharge, but the nature of these symptoms provides important clues. Think of it as being a detective for your own body; every little detail matters.
A classic yeast infection is famous for its thick, white, cottage cheese-like discharge that's typically odorless. BV, on the other hand, often produces a thin, grayish-white discharge along with a distinct, fishy odor that can get stronger after sex. Trichomoniasis can cause a frothy, yellow-green discharge and is often linked to more intense soreness and pain when you pee.
For a definitive answer, a specific Candida Albicans antibody test can offer crucial insights, helping to confirm if the fungus responsible for most yeast infections is truly present.
It's a common misconception that all vaginal discomfort is a yeast infection. In fact, studies have shown that a significant number of women who self-treat for a yeast infection actually have a different condition, such as BV. This highlights why an accurate diagnosis is the most important first step toward effective relief.
A Side-By-Side Comparison
Making sense of these overlapping symptoms gets a whole lot easier when you can see them laid out side-by-side. The table below breaks down the typical signs of these three common conditions. Use it as a guide to better understand what you might be experiencing before you talk to a doctor.
Yeast Infection vs BV vs Trichomoniasis Symptoms
| Symptom | Yeast Infection (Candidiasis) | Bacterial Vaginosis (BV) | Trichomoniasis (STI) |
|---|---|---|---|
| Primary Sensation | Intense itching and burning are the most prominent symptoms. | Mild itching or irritation, but often less intense than a yeast infection. | Significant soreness, itching, and discomfort, often with painful urination. |
| Discharge Texture | Thick, clumpy, and often described as looking like cottage cheese. | Thin, watery, and often grayish-white in color. | Can be frothy or bubbly; may appear yellowish-green. |
| Discharge Odor | Typically odorless, or may have a mild, bread-like scent. | A strong, distinct fishy odor is the classic sign of BV. | Often has a musty or unpleasant odor. |
| Associated Signs | Redness and swelling of the vulva are very common. | Odor is the most noticeable symptom; visible inflammation is less common. | Inflammation, redness, and spotting can occur. |
This comparison really highlights that while the symptoms can feel similar, key differences in discharge texture and odor are powerful clues. For instance, the absence of a strong, fishy smell makes BV less likely, while the presence of a thick, white discharge points more strongly toward a yeast infection. Our guide on bacterial vaginosis dives deeper into this specific condition.
Ultimately, while this guide can help you understand the possibilities, it's no substitute for a professional medical opinion. An accurate diagnosis ensures you get the right treatment—antifungals for yeast, antibiotics for BV or trichomoniasis—so you can find relief faster and avoid the cycle of ineffective self-treatment.
Finding the Right Path to Relief
Once you have a pretty good idea that it's a yeast infection, the next step is getting relief—fast. Navigating the treatment aisle at the pharmacy can feel a little overwhelming, but your options really boil down to two main camps: over-the-counter (OTC) products and prescription medications.
Which path you take depends on a few things: how severe your symptoms are, if this is your first rodeo with a yeast infection, and your overall medical history.
For many women dealing with a classic, uncomplicated yeast infection, the pharmacy is the first and only stop needed. OTC treatments are a convenient and effective way to handle these straightforward cases. These are all antifungal products designed to do one thing: stop the overgrowth of Candida.
Exploring Over-the-Counter Options
When you’re staring at that wall of boxes, you'll see treatments in different forms and for different durations. This isn't just for show; the variety lets you pick a product that fits your comfort level and what you're willing to deal with.
The most common types of OTC antifungals you'll find are:
- Topical Creams: You apply these externally to the vulva to soothe that maddening itch and burn, and internally using an applicator.
- Vaginal Suppositories: These are small, solid capsules (sometimes called ovules) that you insert into the vagina. They dissolve overnight to release the medication right where it's needed.
- Combination Packs: Smart idea. Many brands bundle an internal suppository or cream with a tube of external cream for all-around symptom relief.
You’ll also notice 1-day, 3-day, or 7-day courses. The 1-day options pack a higher, more concentrated dose, while the 3 and 7-day treatments use a lower dose spread out over more time. A single-day dose sounds great, but it doesn't always mean your symptoms vanish in 24 hours. It can still take a few days for everything to calm down, no matter which treatment length you choose.
This decision tree gives you a simple way to think through what you're feeling and figure out if a yeast infection is the likely culprit.
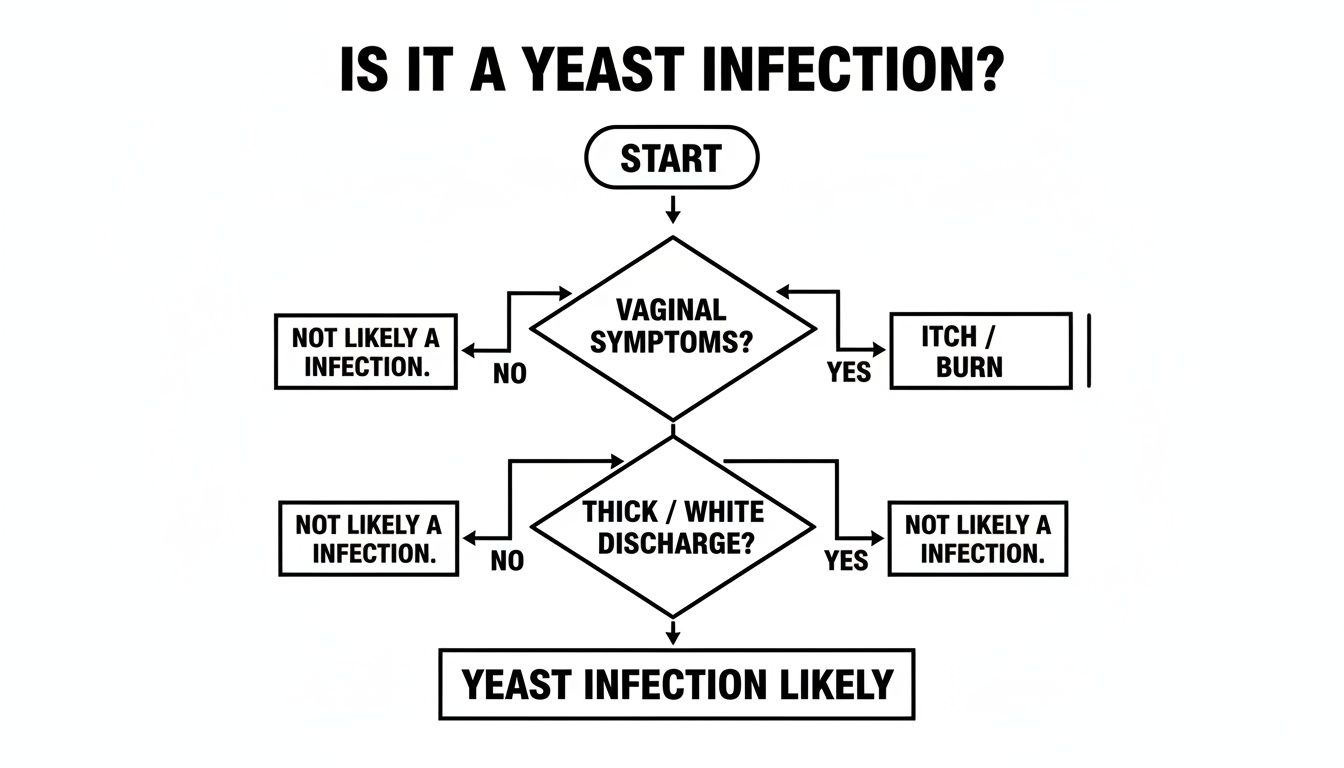
As the flowchart shows, that classic trio of itching, burning, and a thick, white discharge is a strong pointer toward a yeast infection, helping you decide on the next step.
When to Seek a Prescription
While OTC products are fantastic for many, they aren't the right call for everyone. There are definitely times when you need to bring in the bigger guns with a prescription from a healthcare provider. This ensures you get a more potent or targeted treatment when the situation calls for it.
You should always talk to a doctor if:
- This is the very first time you’ve had yeast infection symptoms in women.
- You are pregnant or have an underlying condition like diabetes.
- You’ve had four or more yeast infections in the last year (this is called recurrent candidiasis).
- Your OTC treatment didn't work, or your symptoms came roaring back right after you finished it.
A common mistake is grabbing an OTC kit without being sure it's a yeast infection. If you've used a 7-day treatment and are still miserable, that’s a huge red flag. You might be dealing with something else entirely, like bacterial vaginosis, or a stubborn strain of yeast that just laughs at the OTC stuff.
Prescription options often include stronger topical antifungals or, more commonly, a simple oral antifungal pill. The go-to oral medication is fluconazole, which is usually just a single pill. One and done. It’s a convenient, mess-free alternative to creams, working from the inside out to clear the infection systemically.
Whether you go with an OTC product or need a prescription, the goal is always the same: getting effective, lasting relief. For anyone who needs a quick diagnosis and treatment without the hassle of an in-person visit, getting an online prescription is a fast, private way to connect with a doctor, confirm what's going on, and have a prescription sent straight to your pharmacy.
When Yeast Infections Become a Recurring Problem
Dealing with a single yeast infection is frustrating enough. But for some women, it’s a relentless cycle that just keeps coming back. When that familiar itching and burning return right after you thought you were in the clear, it can feel incredibly disheartening. This isn't just a string of bad luck; it’s a recognized medical condition called recurrent vulvovaginal candidiasis (RVVC).
RVVC is the official term for having four or more yeast infections in a single year. It’s a chronic issue that signals something more persistent is going on than just a simple imbalance. Living with RVVC can seriously mess with your quality of life, leaving you in a state of constant anxiety and discomfort, always waiting for the next flare-up.
Why Do They Keep Coming Back?
Figuring out the "why" behind recurrent infections is the first step toward finally breaking the cycle. It's rarely one single thing but often a combination of factors creating the perfect storm for yeast to thrive again and again. A healthcare provider is your best partner in getting to the root of the problem.
Some of the most common reasons they keep coming back include:
- Resilient Yeast Strains: Not all Candida is created equal. While Candida albicans is the usual suspect, sometimes a less common, more drug-resistant strain is to blame. These stubborn types just don't respond to the standard over-the-counter treatments.
- Underlying Health Conditions: Unmanaged diabetes is a huge contributor, since high blood sugar levels are like a buffet for yeast. Likewise, any condition that weakens your immune system can make it tough for your body to keep yeast populations under control.
- Incomplete Treatment: It's possible a previous infection was never fully knocked out. Using a treatment for too short a time or stopping as soon as you feel better can leave behind lingering yeast cells, ready to multiply all over again.
The numbers around recurrence can be pretty startling. Did you know that nearly half of women who have one yeast infection have a good chance of it becoming a recurring problem? A multinational survey found that over 21% of women went through a 12-month period with four or more episodes, showing just how common this frustrating cycle is. You can learn more about these findings on recurrent yeast infections.
Creating a Long-Term Management Plan
If you feel trapped in a cycle of recurring infections, it's time to stop the self-treating and team up with a healthcare provider. A doctor can confirm the diagnosis, figure out the specific yeast strain causing the trouble, and rule out any other underlying health issues. This professional guidance is essential for creating a long-term strategy that actually works.
Breaking the cycle of recurrent yeast infections requires moving from reactive treatment to a proactive management plan. This often involves a maintenance therapy designed to keep yeast overgrowth at bay before it can cause symptoms.
A common and effective approach for managing RVVC is suppressive therapy. This usually starts with an intensive treatment to clear the current infection, followed by a regular maintenance dose of an antifungal medication. For instance, a provider might prescribe a weekly dose of an oral antifungal pill like fluconazole for six months or even longer. This strategy doesn't just treat the symptoms; it actively prevents the yeast from overgrowing, finally giving your body a chance to restore its natural balance and giving you some long-awaited relief.
Proactive Steps for Preventing Future Infections

Once an infection is gone, the last thing you want is for it to come back. Shifting your focus from treatment to prevention puts you back in the driver's seat of your health. Think of it like tending a garden—the goal is to create an environment where yeast simply can't overgrow in the first place.
These simple, evidence-based habits can make a huge difference in keeping your body's delicate ecosystem in balance and avoiding disruptive yeast infection symptoms in women.
Adjust Your Lifestyle and Wardrobe
Believe it or not, your daily habits and even your clothes can play a huge role in your vaginal health. The name of the game is minimizing moisture and maximizing airflow, since yeast loves warm, damp environments.
A few simple tweaks can have a major impact:
- Choose Breathable Fabrics: Make underwear made from 100% cotton your best friend. Synthetic fabrics like nylon and spandex are notorious for trapping heat and moisture, creating a perfect breeding ground for yeast.
- Avoid Tight-Fitting Clothes: Skinny jeans, leggings, and tight workout gear can also suffocate the area and restrict airflow. When you can, opt for looser-fitting clothing to help things stay dry.
- Change Out of Damp Clothes Promptly: Don't hang around in a wet swimsuit or sweaty gym clothes. Swapping them for something dry as soon as possible is one of the easiest ways to stop moisture from getting trapped against your skin.
These small choices work together to maintain a balanced environment, making it much harder for yeast to take over.
Rethink Your Hygiene Practices
When it comes to vaginal hygiene, "less is more" is almost always the best approach. The vagina is a self-cleaning marvel, and many products marketed to "clean" it can actually disrupt its natural pH balance. This can wipe out the good bacteria that work hard to keep yeast in check.
The goal of vaginal hygiene should be to support the body's natural processes, not to disrupt them. Aggressive cleaning methods and harsh products often do more harm than good by stripping away the protective bacteria essential for a healthy microbiome.
To protect your body's delicate balance, it's best to:
- Steer Clear of Douching: Douching is a definite no. It flushes out the good bacteria needed to control yeast growth. Trust your body's built-in system to stay clean.
- Use Gentle, Unscented Soaps: Harsh, perfumed soaps, bubble baths, and feminine sprays can cause irritation and throw your vaginal pH out of whack. Just stick to warm water or a mild, fragrance-free soap on the external area only.
- Always Wipe from Front to Back: This is a simple but critical habit. It prevents bacteria from the anal region from being introduced to the vagina, which can upset the local microbiome.
Support Your Body from the Inside Out
Your diet and overall health are directly linked to your body's ability to fight off infections. High blood sugar levels, for example, can literally feed yeast and encourage it to multiply. This makes your dietary choices a powerful tool for prevention.
Try to incorporate a balanced diet that's low in processed foods and added sugars. While it isn't a cure, it supports a healthy immune system and a stable internal environment. Some women also find that adding probiotics, like those found in yogurt with live cultures, helps boost their population of beneficial bacteria.
You can learn more about managing different types of yeast and fungal infections with a holistic approach that includes both diet and lifestyle adjustments.
Frequently Asked Questions About Yeast Infections
Even after you've got a handle on the symptoms and treatments, a few questions might still be lingering. That's completely normal when you're trying to figure out what's going on with your body. Here are some clear, straightforward answers to the things women ask about most.
Can I Get a Yeast Infection from My Partner?
This one's a common concern. While a yeast infection isn't technically an STI, it is possible for sexual partners to pass the Candida fungus back and forth. This frustrating cycle, sometimes called "ping-ponging," seems to be more common if a male partner is uncircumcised.
If you keep getting infections no matter what you try, it might be worth talking to a doctor about having your partner checked out. For most women, though, sex isn't the direct cause of a yeast infection.
Does My Diet Really Affect My Risk of Yeast Infections?
Yes, what you eat can definitely play a role, especially if you have trouble with blood sugar control. A diet packed with sugar and refined carbs can essentially feed the yeast, encouraging it to grow out of control.
While super-strict "anti-Candida" diets have some mixed reviews in the science world, a balanced diet that's low in processed sugars is a proven way to support your immune system and keep your vaginal microbiome stable and healthy.
Many women also find that adding probiotics to their routine helps. Think yogurt with live, active cultures or a good quality supplement—they can help maintain that healthy balance of good bacteria.
How Quickly Should I Expect Relief After Starting Treatment?
How fast you'll feel better really depends on how severe the infection is and which treatment you're using. With most over-the-counter or prescription antifungal meds, you should start feeling some relief from the itching and burning within one to three days.
But don't be surprised if it takes up to a full week for every last symptom to disappear completely. If you don't feel any better after a few days—or if things are getting worse—it’s time to call your doctor for a re-evaluation.
Feeling unsure about your symptoms or need a prescription fast? The board-certified physicians at ChatWithDr can provide a private, text-based consultation and send a prescription to your pharmacy in as little as an hour, all for a flat fee. Get the expert care you need without leaving home by visiting ChatWithDr.