Choosing the right birth control is a big deal, and let's be honest, staring at a long list of birth control options and side effects can feel like a lot. This guide is here to cut through the noise. We’ll break everything down so you can feel confident figuring out what works for your body, your lifestyle, and your future.
Your Guide to Navigating Contraceptive Choices

Finding the right birth control is about so much more than just preventing pregnancy—it’s about discovering a method that truly fits into your life. Think of it less like a test you have to pass and more like an honest chat with yourself about your health priorities.
Do you want something you can set and forget? Are you trying to avoid hormones? The answers to these questions are your roadmap.
The world of contraception might seem huge, but it really boils down to just a few main categories. Getting a handle on these groups is the first big step toward finding your perfect match.
The Main Categories of Birth Control
Every type of birth control works a little differently, with its own unique set of pros and cons. The goal is to find one that aligns with what matters most to you. For some, convenience is everything. For others, it might be about managing period pain or sticking to hormone-free options.
To give you a clearer picture, let's look at a summary of the main categories and what they offer.
Birth Control Methods at a Glance
| Category | Examples | Effectiveness (Typical Use) |
|---|---|---|
| Hormonal | Pills, Patch, Ring, Shot, Implant, Hormonal IUD | 91% – 99%+ |
| Hormone-Free & Barrier | Copper IUD, Condoms, Diaphragm, Cervical Cap | 76% – 98% |
| Permanent | Tubal Ligation (for women), Vasectomy (for men) | >99% |
| Fertility Awareness | Symptom-thermal, Calendar, Cervical Mucus | 76% – 99% |
This table provides a quick overview, but remember that the "best" method is the one that you can use consistently and that fits your health and life plans.
The right method for you is one that you can use consistently and correctly, and that aligns with your health profile and life plans. Discussing these factors with a healthcare provider is a critical step in making an informed choice.
Talking this through with a professional is a crucial part of the process. If you're looking for an easy, private way to get medical advice, telehealth services can connect you with a clinician for same-day care right from home. It’s a great way to ask all your questions and get personalized recommendations without the hassle of an office visit.
How Hormonal Birth Control Methods Work

Hormonal birth control is an incredibly popular and effective way to prevent pregnancy, used by millions of people across the globe. Think of it as a clever way of using your body's own communication system—hormones—to gently press pause on fertility. These methods introduce synthetic versions of hormones like estrogen and progestin to guide your reproductive cycle.
The main goal is simple: to stop ovulation. That’s the monthly release of an egg from your ovaries. If there’s no egg, pregnancy just can't happen.
But there's a backup plan, too. These hormones also thicken the mucus around your cervix, creating a natural barrier that makes it much tougher for sperm to get through. This one-two punch is what makes hormonal methods so reliable when used correctly.
Combined Hormonal Methods: The Pill, Patch, and Ring
The most familiar types of hormonal birth control are combined methods, which contain both estrogen and progestin. This category includes the daily birth control pill, the weekly patch, and the monthly vaginal ring. They all deliver hormones in slightly different ways, but they work the same way inside your body.
The pill is taken every day, the patch gets swapped out once a week, and the ring is replaced every month. This steady supply of hormones keeps your body in a state that prevents the hormonal surge needed for ovulation.
Beyond preventing pregnancy, many people turn to these methods for some welcome health perks.
- Lighter, More Predictable Periods: They can be a game-changer for reducing heavy bleeding and painful menstrual cramps.
- Clearer Skin: Many users find that their hormonal acne starts to clear up.
- Lower Cancer Risk: Long-term use has been linked to a reduced risk of both ovarian and endometrial cancers.
Of course, introducing new hormones can bring some unwelcome side effects, especially in the first few months while your body adjusts. It's common to experience things like nausea, breast tenderness, bloating, and mood changes. For most people, these issues fade away over time.
Progestin-Only Options: The Mini-Pill, Shot, Implant, and Hormonal IUD
For anyone who can't take estrogen—perhaps due to a history of blood clots, certain types of migraines, or being over 35 and a smoker—progestin-only methods are a fantastic alternative. This group includes the "mini-pill," the shot (Depo-Provera), the implant (Nexplanon), and hormonal IUDs (like Mirena or Kyleena).
These methods work primarily by thickening cervical mucus to block sperm. Some may also stop ovulation, but it’s not always their main job. The mini-pill, for instance, has to be taken at the exact same time every single day to be effective.
In contrast, long-acting reversible contraceptives (LARCs) like the implant and hormonal IUDs offer a "set it and forget it" kind of freedom.
- The Implant: A tiny, flexible rod placed in your arm that releases progestin for up to three years.
- Hormonal IUDs: A small, T-shaped device placed in the uterus that releases progestin for three to eight years, depending on the brand.
These options are over 99% effective because they take human error out of the equation. The shot is another option, but it requires a visit to your clinician every three months. Side effects for progestin-only methods often involve changes to your period, like irregular spotting or your period stopping completely.
Choosing a hormonal method means finding the right balance for your body. The adjustment period can take up to three months, so patience is key. If side effects persist, it doesn't mean hormonal birth control isn't for you—it might just mean a different formulation or delivery method is a better fit.
Potential Side Effects and What to Expect
When you're exploring birth control options and side effects, it's important to have a realistic picture. While many people have no issues at all, others find the initial adjustment period a bit challenging.
Here are some common side effects you might notice at first:
- Irregular Bleeding or Spotting: This is incredibly common in the first three to six months as your body gets used to the new hormone levels.
- Nausea: Taking the pill with a snack or right before bed can often help with this.
- Headaches: These are usually mild and tend to go away on their own.
- Mood Shifts: Some people report feeling more emotional or irritable as their body adjusts.
More serious, though rare, risks are associated with methods that contain estrogen, mainly a small increased risk of blood clots. This risk is highest for people who smoke, are over 35, or have a personal or family history of blood clots. It's crucial to share your complete medical history with your healthcare provider.
The global reliance on contraception highlights its critical role in health and wellness. In the U.S., long-acting reversible contraception (LARC) like IUDs accounts for 10.4% of use, reflecting a shift toward highly reliable options. This is part of a massive worldwide effort, with an estimated 874 million women using modern contraceptive methods as of 2022, a number that continues to grow. You can discover more birth control trends and statistics from SingleCare's detailed report.
While on hormonal birth control, understanding how to support your body's natural balance can make a big difference. It's helpful to learn about ways to manage your well-being, and you might explore how to use supplements to balance hormones effectively. Finding what works for your unique body is the most important part of this journey.
Exploring Hormone-Free and Barrier Methods

If you're looking for a way to prevent pregnancy without changing your body's natural hormonal cycle, you have some fantastic options. Hormone-free methods work with your body, not against it, offering solid protection for anyone who’d rather skip synthetic hormones for personal or medical reasons.
These choices range from long-term, “set it and forget it” devices to methods you only use when you have sex. Let’s dive into the world of non-hormonal birth control options and side effects, starting with one of the most effective methods out there.
The Copper IUD: A Long-Term Solution
The copper IUD, known in the U.S. by the brand name ParaGard, is a real powerhouse in the world of hormone-free birth control. It’s a tiny, T-shaped device that’s gently wrapped in a bit of copper wire. A clinician places it in your uterus during a quick office visit.
So how does it work without hormones? The copper itself creates an environment where sperm simply can’t survive, stopping fertilization in its tracks. It's an incredibly reliable method, with an effectiveness rate of over 99%.
One of its biggest draws is how long it lasts. Once it’s in place, it can prevent pregnancy for up to 10 years. It truly is a "set it and forget it" option.
Did you know the copper IUD is also the most effective form of emergency contraception available? If a clinician inserts it within five days of unprotected sex, it’s more than 99.9% effective at preventing a pregnancy.
Of course, like anything, there are potential downsides. The most common side effects are heavier, longer, and more crampy periods, particularly in the first few months. While this usually gets better with time, it’s a big consideration if your periods are already difficult.
Barrier Methods: Putting a Block on Pregnancy
Barrier methods do exactly what their name suggests—they create a physical wall that stops sperm from getting to an egg. These are “on-demand” methods, meaning you only use them right when you’re having sex. They’re a great choice if you want something you control in the moment without a long-term commitment.
The key to making barrier methods work is using them correctly and consistently, every single time. Unlike an IUD that works on its own, their effectiveness is completely in your hands.
Let’s walk through the most common types.
Condoms: The Only Dual-Protection Method
Condoms, both external (male) and internal (female), are in a class of their own. They are the only birth control method that also protects you from sexually transmitted infections (STIs). With typical, real-world use, external condoms are about 87% effective, while internal condoms are around 79% effective.
- Pros: Easy to find, affordable, and they provide that crucial STI protection.
- Cons: They can break or slip if not used correctly, and some people are sensitive to latex (though latex-free versions are widely available). Their success rate is all about proper use.
Diaphragms and Cervical Caps: A Personal Fit
A diaphragm is a small, shallow silicone cup, while a cervical cap is even smaller and shaped like a thimble. You insert either one into your vagina before sex to cover your cervix. For them to work, you have to use them with spermicide.
You'll need a prescription to get one, as a clinician needs to make sure you have the right size and show you how to put it in and take it out correctly. With typical use, their effectiveness is between 76% to 83%.
- Pros: You can put one in hours before sex, which allows for more spontaneity. They are also reusable and hormone-free.
- Cons: Getting the hang of inserting and removing them can be tricky. You also have to leave them in for at least six hours after sex, and some people find that the required spermicide causes irritation.
Choosing Your Hormone-Free Path
Deciding on the right hormone-free method really comes down to what you value most: effectiveness, convenience, or comfort. The copper IUD gives you top-tier, long-lasting protection but might make your periods tougher. Barrier methods offer on-demand control and STI protection (with condoms), but their success is entirely dependent on you.
Think about your lifestyle and what’s most important to you. Are you looking for something you won’t have to think about for years? Or do you prefer a method you only use when you need it?
Thinking through these birth control options and side effects is the most important step. Chatting with a clinician can help you sort through it all, ensuring you find a method that not only prevents pregnancy but truly fits into your life.
Permanent and Natural Options: A Different Approach
When you’ve reached a certain point in life or have a different philosophy on family planning, the birth control conversation can shift away from hormones and barrier methods. This often leads people down two very distinct paths: permanent surgical procedures or highly involved natural techniques.
Both of these routes require a serious level of commitment and a deep understanding of what you’re signing up for, but they can be the perfect fit for the right person.
Permanent methods, like vasectomies and tubal ligations, are for people who are absolutely certain they don’t want any more children. These surgical procedures are more than 99% effective, offering a "one-and-done" solution that you never have to think about again.
On the other end of the spectrum, you have Fertility Awareness-Based Methods (FABMs). These are completely natural and hormone-free, but their success hangs entirely on you becoming an expert at tracking your body’s fertility signals. And you have to do it consistently.
Permanent Birth Control: A Lifelong Decision
Choosing to get sterilized is a big deal and requires a lot of careful thought and counseling. It’s not just a medical procedure; it’s a final decision about your future family plans.
A vasectomy is a pretty simple outpatient procedure for men. A provider cuts or blocks the tubes that carry sperm, known as the vas deferens. It's much less invasive than female sterilization and the recovery time is quicker. While it’s incredibly effective, it’s not instant—it can take a few months to fully clear sperm from the system.
Tubal ligation is the surgical option for women. The fallopian tubes are either cut, blocked, or removed to stop an egg from ever reaching the uterus. It’s a more involved surgery, usually done laparoscopically, and it's also over 99% effective.
You may have heard that these procedures can be reversed. While it’s technically possible in some cases, reversal surgeries are incredibly complex, expensive, and there's no guarantee they'll restore your fertility. It’s best to go into this thinking of it as a final step.
Fertility Awareness-Based Methods (FABMs)
Often called natural family planning, Fertility Awareness-Based Methods (FABMs) are a world away from permanent procedures. Instead of a one-time surgery, FABMs demand daily attention and a real dedication to understanding your menstrual cycle. It’s all about tracking your body's natural signs to pinpoint which days you're fertile and which you aren't.
To make this work, you have to become a pro at tracking several key indicators:
- Basal Body Temperature: This is your body's temperature when you’re fully at rest. It rises just slightly after you ovulate.
- Cervical Mucus: The texture and consistency of your cervical mucus change throughout your cycle. It becomes clear, stretchy, and slippery—like egg whites—when you’re most fertile.
- Cervical Position: The position and feel of your cervix can also shift, giving you another clue about your fertility window.
This isn’t just a guessing game; it’s a science that requires precision. If you do it perfectly, every single time, FABMs can be up to 99% effective. But in the real world, with typical use, that effectiveness drops to around 76-88%. There's just a lot of room for human error.
Is FABM the Right Fit for You?
This method really works best for people in stable relationships who have regular cycles and are incredibly motivated to track their symptoms every single day. It also requires buy-in from both partners, since you’ll need to use a barrier method or avoid sex during fertile days—which can be a week or more each month.
The huge plus is that it's completely natural. No hormones, no devices, just you and the rhythm of your body. The biggest downside is the lower "typical use" effectiveness and the sheer amount of daily diligence it takes. If your schedule is unpredictable or you're not a stickler for details, this might not be your most reliable choice. Understanding all your birth control options and side effects means being honest with yourself about whether this high-involvement method truly fits your life.
How to Find the Right Birth Control for You
Trying to navigate the world of contraception can feel like learning a whole new language. With so many birth control options and side effects on the table, picking one can feel overwhelming. The secret is to stop looking for the single "best" method out there and start focusing on the best method for you.
This really just means taking a good, honest look at your life, your health, and what you’re comfortable with. Think of it as a personal checklist that helps you match a birth control option to your unique situation. When you do that, the final decision feels less like a shot in the dark and more like a choice you can stand behind.
Start With Your Lifestyle and Daily Habits
Your day-to-day routine is one of the biggest clues to which birth control will actually work for you. Are you the kind of person who thrives on a schedule, or do you need something you can set and forget? Just answering that one question can immediately narrow your options.
Here are a few things to think about:
- Memory and Routine: Are you confident you can take a pill at the exact same time every single day? If that sounds like a stretch, a weekly patch, monthly ring, or a long-acting method like an IUD or the implant might be a much better fit.
- Spontaneity: Do you prefer contraception that doesn’t require you to stop and think in the moment? Methods like condoms or diaphragms need to be used right before sex, while an IUD or implant is working 24/7 in the background.
- Comfort Level: How do you feel about medical procedures? The idea of having an IUD inserted might be a non-starter for some, who would much prefer a non-invasive option like the pill.
Getting real with yourself about these lifestyle factors helps you quickly weed out the options that just aren’t going to stick.
Evaluate Your Health History and Future Plans
Your health background is a critical piece of the puzzle, and there’s no room for guesswork here. Some medical conditions can make hormonal methods—especially those with estrogen—risky. That’s why it’s so important to be completely open with your clinician about your medical history.
Key health factors include:
- Medical Conditions: A history of blood clots, certain kinds of migraines (especially migraine with aura), high blood pressure, or breast cancer can rule out birth control with both estrogen and progestin.
- Smoking: If you are over 35 and you smoke, estrogen-containing birth control is generally off the table due to a higher risk of blood clots.
- Future Family Plans: Are kids in your future? If so, when? Most methods are easily reversible, but some, like the Depo-Provera shot, can come with a longer delay before your fertility returns to normal after you stop.
This decision tree can help you see how these choices play out when you're considering a long-term birth control option.
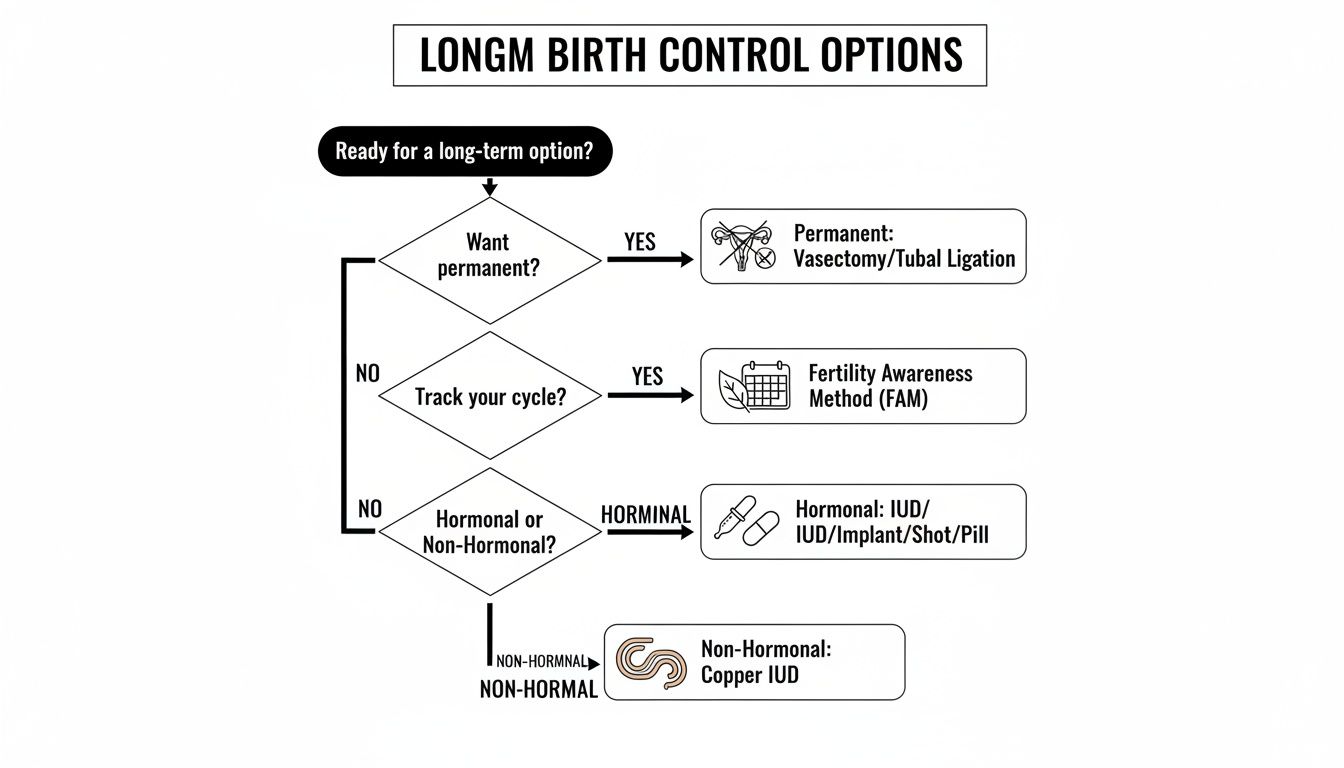
As you can see, just answering a few questions about how permanent you want your method to be and whether you want hormones can point you in the right direction.
Weighing the Emotional and Financial Factors
The effects of birth control aren’t just physical. For some people, hormonal methods can impact their mood, and it's good to be aware of that possibility. If you're weighing your options, it's smart to know that side effects can sometimes include anxiety. If you ever experience this, having resources on strategies for managing anxiety can be a huge help.
Cost is another real-world factor. Some methods like an IUD have a higher price tag upfront, but they can end up being cheaper over several years compared to buying pills or patches every month.
Your perfect birth control method sits at the intersection of effectiveness, convenience, safety, and cost. The goal is to find something you can use consistently and correctly, with side effects you can live with.
Ultimately, thinking through these questions prepares you for a really productive chat with a healthcare provider. Services that offer online birth control consultations can make this step incredibly easy, letting you talk through your specific needs and get a prescription without leaving home. By doing a little self-reflection beforehand, you can go into that conversation ready to make a great decision for your reproductive health.
Comparing Popular Birth Control Options
To help you see how different methods stack up, we've put together a table comparing some of the most common options. This isn't an exhaustive list, but it's a great starting point for seeing the trade-offs between effectiveness, side effects, and what's required of you.
| Method | Effectiveness (Typical Use) | Common Side Effects | User Action Required | Upfront Cost |
|---|---|---|---|---|
| Pill (Combination) | 93% | Nausea, breast tenderness, mood changes, spotting | Take daily at the same time | $0–$50/month |
| IUD (Hormonal) | 99.8% | Irregular bleeding, cramping, lighter or no periods | One-time insertion by a clinician (lasts 3-8 years) | $0–$1,300 |
| IUD (Copper) | 99.2% | Heavier periods, cramping, spotting | One-time insertion by a clinician (lasts up to 12 years) | $0–$1,300 |
| Implant | 99.95% | Irregular bleeding, headaches, mood changes | One-time insertion by a clinician (lasts up to 5 years) | $0–$1,300 |
| Shot (Depo-Provera) | 96% | Irregular bleeding, weight gain, delayed return to fertility | Injection from a clinician every 3 months | $0–$150/injection |
| Male Condom | 87% | Latex allergy (rare) | Use correctly every time you have sex | ~$1 each |
Remember, "typical use" effectiveness rates account for human error—like forgetting a pill or using a condom incorrectly. This table should help you start a conversation with your provider about what might be the best match for your body and your life.
Common Questions About Birth Control
Diving into the world of birth control can feel a little overwhelming, and it’s totally normal to have a few “what if” questions pop up. Once you’ve learned about all the different options, a few things might still feel unclear. Let's walk through some of the most common concerns to help you feel confident and in control of your reproductive health.
How Does Emergency Contraception Work
Emergency contraception (EC), often called the “morning-after pill,” is a safe backup plan to prevent pregnancy after you’ve had unprotected sex. Its main job is to stop or delay ovulation, which means it prevents your ovary from releasing an egg. If there’s no egg, sperm has nothing to fertilize.
It's important to know that EC is not an abortion pill. It won't work if you're already pregnant, and it won't harm an existing pregnancy.
There are a few different kinds you can get:
- Levonorgestrel pills (like Plan B): These are most effective when you take them within 72 hours (that’s 3 days) of unprotected sex. You can find them over the counter.
- Ulipristal acetate pills (ella): This type works for up to 120 hours (5 days) but you’ll need a prescription to get it.
- Copper IUD: If a clinician inserts a copper IUD within 5 days, it’s actually the most effective EC out there—over 99.9% effective, in fact.
Just remember, EC is meant for emergencies, not as your regular go-to birth control method. The sooner you use it, the better it works.
Will Birth Control Affect My Future Fertility
This is probably one of the biggest worries we hear, and the good news is that for almost everyone, using birth control has no impact on your ability to get pregnant later. Once you stop methods like the pill, patch, or ring, or have an IUD or implant removed, your body’s natural cycle usually bounces back within a few months.
Think of it like pausing a movie. When you’re ready, you just hit play again, and the story continues right where it left off. If you do experience delays in getting pregnant after stopping contraception, it's typically due to the same underlying factors that were there before you started. The only methods that permanently change your fertility are sterilization procedures.
Your body is resilient. Most contraceptive methods are designed to be fully reversible, allowing your natural fertility to return shortly after you stop using them. Patience is key as your cycle readjusts.
What Should I Do If I Experience Side Effects
When you start a new hormonal birth control, it's really common to go through an adjustment period. For the first three months or so, your body is getting used to the new hormone levels, so you might notice things like spotting, mild headaches, or mood shifts.
But you shouldn't have to just "tough it out" if the side effects feel severe, don't go away, or are seriously impacting your quality of life. That's your cue to reach out to a healthcare provider. They can help you figure out if what you’re feeling is a normal part of the adjustment or if trying a different method would be a better fit.
Some symptoms are more urgent. If you ever experience severe chest pain, shortness of breath, or sudden, severe leg pain, get medical attention right away. These can be signs of a rare but serious issue like a blood clot.
At the end of the day, you have to advocate for yourself. The right birth control should fit into your life without making you feel awful. For more answers, you can also check out this detailed list of frequently asked questions about reproductive health.