When you’re stuck with that deep, hacking cough and miserable chest congestion, the first question on your mind is always the same: how long is this going to last? For most cases of acute bronchitis, the worst of it—like the fever and body aches—usually gets better within 3 to 10 days. But that nagging cough? That can stick around for several weeks while your airways heal.
A Clear Timeline for Your Bronchitis Recovery
Knowing what to expect from the recovery process can make a world of difference. It helps you set realistic expectations and dials down the anxiety when that cough just won’t quit.
Think of your airways like a path that’s been roughed up by a storm. The storm itself (the initial viral infection) passes relatively quickly, but the path is still damaged and needs time for repairs. That’s why the cough sticks around long after you start feeling more like yourself again.
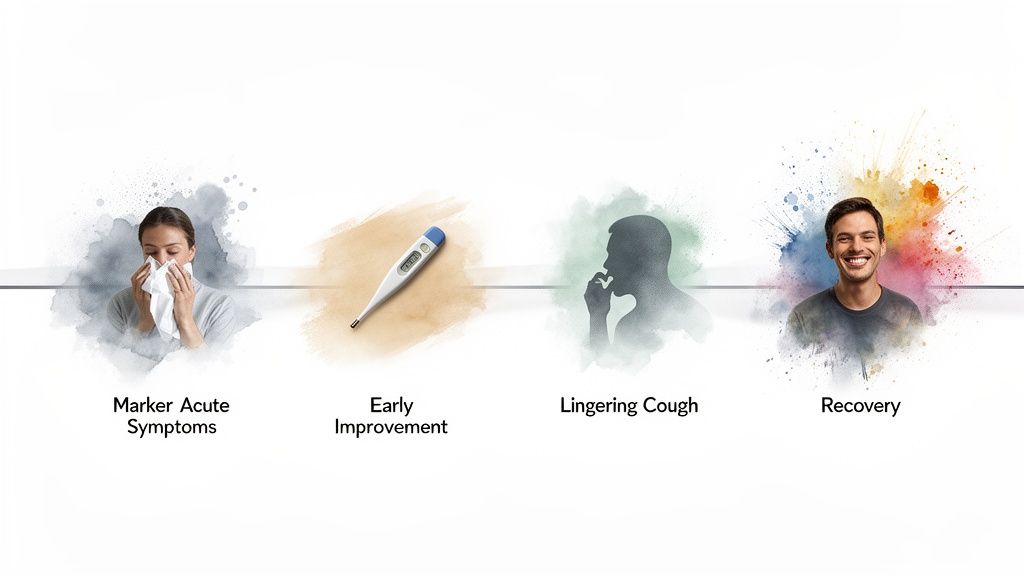
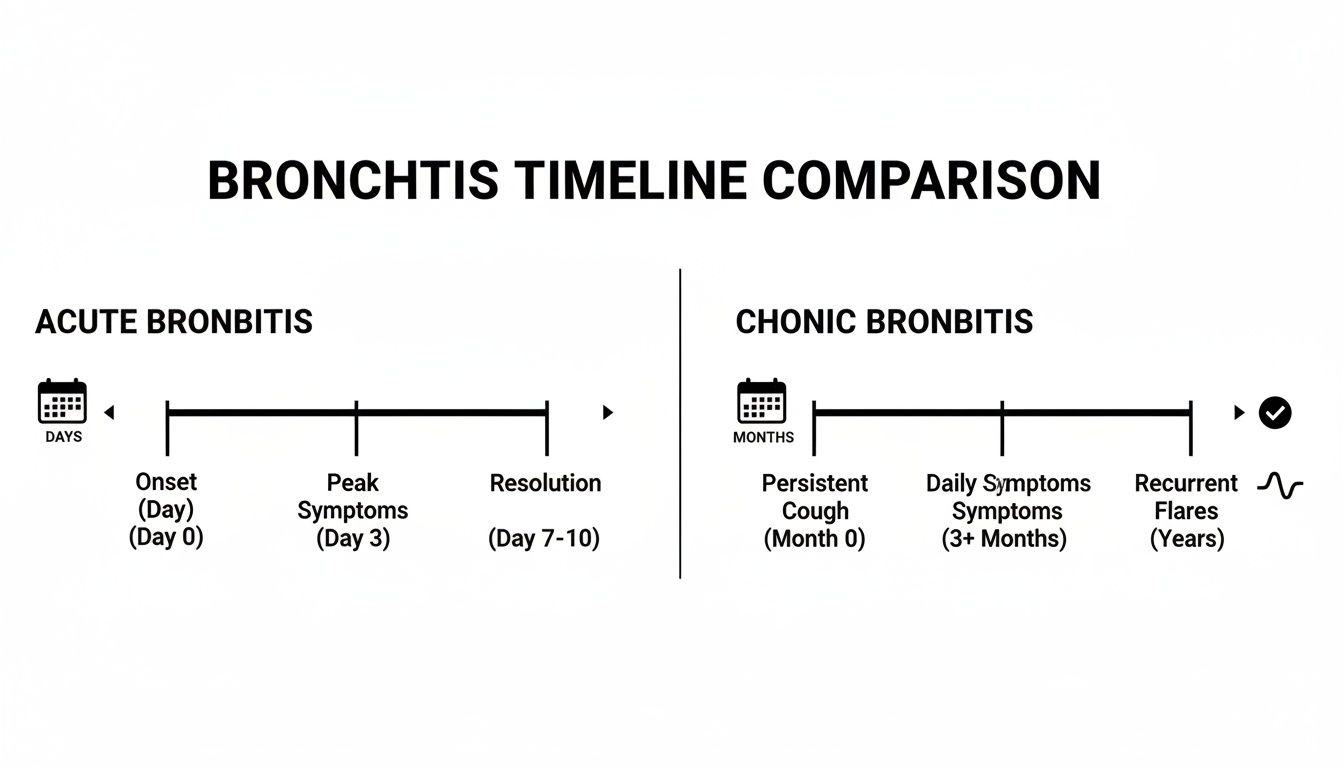
To give you a clearer picture, let's break down what a typical timeline looks like for both acute and chronic bronchitis. This quick-reference table provides a straightforward overview of what to expect, from the first signs of illness to when that lingering cough should finally fade.
Bronchitis Duration at a Glance
| Type of Bronchitis | Initial Symptom Duration | Lingering Cough Duration | When to Expect Improvement |
|---|---|---|---|
| Acute Bronchitis | 3 to 10 days | Up to 3-4 weeks (sometimes longer) | Within the first week |
| Chronic Bronchitis | Ongoing (symptoms for 3+ months for 2+ years) | Persistent, long-term cough | Varies with treatment and triggers |
It's important to remember that this is just a general guide. Your personal timeline can be influenced by a handful of different factors.
Your overall health, age, and whether you smoke can all impact how quickly your body heals from bronchitis. A healthy immune system can clear the initial infection faster, but the airway inflammation may still follow a similar healing course.
This difference is key because it explains why two people with the exact same illness can have very different recovery experiences. Later on, we’ll dig into why distinguishing between acute and chronic forms is the crucial first step toward understanding your specific situation and finding the right path to relief.
Acute vs Chronic Bronchitis Explained
To figure out how long your recovery might take, you first have to know what kind of bronchitis you’re up against. Think of acute bronchitis as a sudden, nasty storm—it rolls in, causes a lot of disruption, and then it passes. Chronic bronchitis, on the other hand, is like a heavy fog that just won’t lift, lingering for months or coming back again and again.
Telling them apart is the most important first step. It shapes everything from how long you can expect to feel sick to the right way to treat it. While they share a name, they’re two very different conditions with different causes, timelines, and game plans for getting better.
The Short-Term Intruder: Acute Bronchitis
Acute bronchitis is almost always the aftermath of a viral infection, usually showing up right after a common cold or the flu. This is what most people mean when they say they have "bronchitis." It hits you hard and fast, makes you feel pretty miserable, and then your body fights it off. If you're trying to tell the difference, our guide on the cold, flu, and COVID can help clear things up.
The typical journey starts with cold symptoms that quickly sink into your chest, bringing on that classic deep, hacking cough. Most of the sickness feeling goes away in about a week, but the cough often sticks around because your airways need more time to heal from all the inflammation. While the worst of acute bronchitis is usually over in 3 to 10 days, don't be surprised if that cough hangs on for 3 weeks or even longer. For more on this, you can learn about bronchitis recovery timelines from Medical News Today.
The Long-Term Condition: Chronic Bronchitis
Chronic bronchitis isn’t just a temporary bug; it’s a serious, long-term medical condition and a form of chronic obstructive pulmonary disease (COPD). The official definition is having a productive (mucus-producing) cough for at least three months of the year, for two years in a row.
Unlike its short-term cousin, chronic bronchitis is rarely caused by an infection. It’s the result of long-term damage to the airways from constant irritation.
The number one cause of chronic bronchitis is cigarette smoking. Other culprits include secondhand smoke, air pollution, and breathing in dust or chemical fumes at work. This ongoing irritation leads to constant inflammation and an overproduction of mucus.
To make things crystal clear, this table breaks down the key differences at a glance. It should help you get a better sense of which path you might be on.
Acute Bronchitis vs Chronic Bronchitis
| Feature | Acute Bronchitis | Chronic Bronchitis |
|---|---|---|
| Primary Cause | Viral infection (e.g., cold/flu) | Long-term exposure to irritants (smoking) |
| Onset | Sudden and follows a cold | Gradual and develops over years |
| Symptom Duration | A few weeks | Long-term, recurring over months and years |
| Nature | A temporary illness that resolves | A permanent, chronic condition (COPD) |
| Treatment Goal | Symptom relief while the body heals | Managing symptoms and slowing disease progression |
Understanding this distinction is crucial because the approach to feeling better is completely different for each one. One requires rest and time, while the other demands a long-term management plan with your doctor.
Your Week-by-Week Symptom Guide
When you're sick, knowing what to expect can make the whole ordeal feel a lot less overwhelming. With acute bronchitis, the recovery journey usually follows a pretty predictable path, even if it feels like it's dragging on forever. Understanding the timeline helps you see that a nagging cough is just a normal part of your body healing.
Think of it like a sprained ankle. The sharp, initial pain fades, but the joint stays weak and sensitive for a while as it slowly regains its strength. Your airways are no different—they need time to heal long after the virus or bacteria that caused the infection is gone.
Week One: The Peak of Symptoms
The first week is almost always the toughest. It usually kicks off with all the familiar signs of a nasty cold or upper respiratory infection.
- A sore, scratchy throat and a stuffy nose.
- A low-grade fever that leaves you feeling achy all over.
- That classic run-down, fatigued feeling.
A few days in, the infection usually makes its way down into your chest. This is when the signature bronchitis cough shows up. It often starts as a dry, hacking irritation before becoming productive—meaning you start coughing up mucus. Don't be surprised if your chest feels sore and tender from all the coughing. That's completely normal at this stage.
This timeline shows how acute bronchitis is a short-term fight, while its chronic counterpart is a long-haul condition.
As you can see, acute bronchitis is measured in weeks, not the months or years that define the chronic version.
Week Two: You're Turning a Corner
By the second week, you should really start to feel some relief. The fever, body aches, and that crushing fatigue usually back off, and you'll start feeling more like yourself again. But one symptom is going to stick around.
Your cough will still be front and center, and it will likely be very productive. This is actually a good thing. The inflammation in your bronchial tubes is finally calming down, and your body is in full clean-up mode, working hard to expel all the mucus that built up during the infection. It’s annoying, but it’s a clear sign of healing.
Key Takeaway: It's standard to feel much better overall while still dealing with a persistent, mucus-producing cough. The cough is the last symptom to go because your airways took the biggest hit and need the most time to repair themselves.
Weeks Three and Beyond: The Lingering Cough
This is the part that throws most people off. You feel fine, you’re back at work, but that cough just won’t let go. A post-bronchitis cough can easily hang around for three to four weeks, and in some cases, up to eight weeks after the initial illness has passed.
Why? Because your bronchial tubes are still incredibly sensitive from all that inflammation. Things that wouldn't have bothered you before can now trigger a coughing fit in an instant:
- Taking a deep breath of cold air
- Laughing too hard or even just talking a lot
- A whiff of dust, perfume, or other strong scents
Patience is your best friend during this final phase. Your airways are finishing their repair work, and the cough will slowly become less frequent and less intense until it finally fades away completely. If the cough gets worse or is still going strong after a month with no signs of improvement, it’s a good idea to check in with a healthcare provider.
Factors That Can Delay Your Recovery
While most cases of acute bronchitis stick to a fairly predictable timeline, some people find their cough and fatigue just won't quit. If it feels like your recovery is dragging on, certain underlying factors could be pumping the brakes on the healing process. Understanding these can help explain why your body might need a little extra time to get back on its feet.
Think of it like this: your body’s recovery is a construction project. If you have all the right materials and a solid foundation, everything goes smoothly. But if that foundation is shaky or there are constant disruptions, the whole project is going to take much, much longer.
Underlying Health Conditions
Your overall health is the foundation of your recovery. Certain pre-existing conditions can make it much harder for your body to fight off the inflammation bronchitis leaves behind.
- Asthma: If you have asthma, your airways are already sensitive and prone to inflammation. Bronchitis just adds fuel to that fire, often triggering more severe symptoms and a cough that lingers for weeks. You can learn more about how asthma interacts with respiratory illnesses in our detailed guide.
- Weakened Immune System: Conditions that compromise your immune system—or treatments like chemotherapy—leave your body with fewer soldiers to fight the infection and repair the damage. This can stretch out the recovery timeline significantly.
- GERD (Acid Reflux): It might sound unrelated, but chronic acid reflux can constantly irritate your throat and airways. This makes them more susceptible to inflammation and can absolutely prolong that nagging bronchitis cough.
For many, the cough from bronchitis is the last symptom to leave the party. It often sticks around for 3-6 weeks even after other symptoms fade because the irritated airways need that much time to fully clear out mucus and rebuild. To understand more, discover insights on bronchitis recovery from Liv Hospital.
Lifestyle and Environmental Factors
Your daily habits and your environment have a huge impact on how fast you heal. Some choices can actively work against your body's best efforts, turning a simple recovery into an uphill battle.
The single biggest offender? Smoking. Trying to get over bronchitis while you're still smoking is like trying to put out a fire while someone keeps tossing matches on it. The smoke constantly irritates your already-inflamed airways, preventing them from healing and making you a prime target for secondary infections.
Other factors like your age can also play a role. The very young and older adults often have a tougher time clearing the infection, which can lead to a longer illness. And don't underestimate the power of rest. Pushing yourself too hard diverts precious energy that your body needs for healing, effectively delaying the entire process. Recognizing these roadblocks is the first step to clearing them out of your way.
Speeding Up Recovery and When to See a Doctor

While your body does most of the heavy lifting to clear bronchitis, you can definitely give it a helping hand. Simple, consistent self-care can soothe your symptoms and help you feel better, faster. Think of it as creating the perfect environment for your body to do its repair work without any distractions.
First up is hydration. This one is non-negotiable. Drinking plenty of fluids like water, herbal tea, or clear broth helps thin the mucus clogging up your airways, making it much easier to cough up and clear out. It’s one of the most effective ways to make your cough less exhausting and more productive.
Right alongside hydration is rest. Your immune system burns a ton of energy fighting off an infection and healing that inflamed tissue. Trying to push through your fatigue just steals resources from the healing process and can actually make your recovery take longer. Giving your body the downtime it’s demanding is a critical part of getting well.
Creating a Soothing Environment
You can also tweak your surroundings to make them more healing-friendly. Running a cool-mist humidifier or vaporizer adds moisture to the air you're breathing, which helps keep your airways from drying out and getting even more irritated. This is a game-changer at night for cutting down on coughing fits so you can get some decent sleep.
Some people also look into complementary approaches to feel better. While your doctor's advice should always come first, things like understanding how to approach using a sauna when sick can be part of a guided recovery plan for some. Just make sure you talk to a healthcare professional before trying any new wellness strategies while you're sick.
These home care tactics are great for supporting your body, but you also need to know when self-care just isn't cutting it.
Red Flags That Mean It's Time for a Doctor
Most cases of acute bronchitis go away on their own with a bit of time and rest. However, some symptoms are red flags telling you it’s time to stop guessing and get professional medical advice. A lingering cough is pretty normal, but certain signs can point to a complication like pneumonia or a secondary bacterial infection setting in.
A cough that lasts more than three to four weeks without getting any better is a big reason to see a doctor. A post-bronchitis cough can stick around for a while, but one that’s just not fading might signal another underlying issue.
Be on the lookout for these specific warning signs that call for a medical evaluation:
- A High or Persistent Fever: A fever that hangs on for more than a few days, or one that spikes above 100.4°F (38°C), suggests your body might be fighting something more serious than a simple virus.
- Difficulty Breathing: Feeling short of breath, wheezing, or having chest pain are not typical for uncomplicated bronchitis and need immediate attention.
- Discolored Mucus: While some yellow or green mucus can be normal, if it comes with a worsening cough or a fever, it could mean you've developed a bacterial infection.
- Coughing Up Blood: Even a tiny amount of blood in your mucus is a clear signal to contact a healthcare provider right away.
When these symptoms pop up, getting a proper diagnosis is crucial. A doctor can rule out more serious conditions and make sure you're on the right treatment plan. For a quick and easy evaluation without leaving your couch, you can get help through an online urgent care provider who can assess your symptoms and tell you what to do next.
Still Have Questions About Your Bronchitis Recovery?
Even with a clear timeline in mind, it's totally normal to have a few nagging questions about what to expect as you get better. We get it. Feeling sick is stressful enough without having to guess about the details.
Think of this section as your go-to guide for those specific concerns that pop up while you're on the mend. We'll cover everything from whether you can pass it on to your family to why that cough just sounds… different.
Am I Contagious and for How Long?
This is easily one of the most common—and important—questions people ask. The answer really depends on what caused your bronchitis in the first place.
For the vast majority of people (over 90% of acute bronchitis cases), the illness was kicked off by a virus. In that case, yes, the virus itself is contagious. You're typically spreading germs for several days up to a week, especially when you have symptoms like a fever and body aches. It's the cold or flu virus you're passing along, not "bronchitis" itself. Once those initial symptoms fade, you're generally not contagious anymore, even if the cough decides to stick around.
On the other hand, if you have chronic bronchitis caused by long-term irritants like smoking, it's not contagious at all. There’s no bug to spread.
Will I Need Antibiotics for Bronchitis?
The short answer here is almost certainly no. Since most acute bronchitis is viral, antibiotics are completely useless. They're designed to fight bacteria, not viruses, so taking them won't help you recover any faster.
In fact, popping antibiotics when they aren't needed can cause unpleasant side effects and contributes to the massive global problem of antibiotic resistance. A doctor will only prescribe them if they have a good reason to think a secondary bacterial infection has set in. This is pretty rare, but might be suspected if you have a high fever that won't break or if you suddenly get much worse after starting to feel better.
A professional diagnosis is crucial. Never self-prescribe or use leftover antibiotics from a previous illness. A healthcare provider can figure out the real cause of your sickness and get you on the right track.
Can Bronchitis Turn into Pneumonia?
Yes, it's possible for bronchitis to progress into pneumonia, but it's an uncommon complication, especially for healthy adults. Pneumonia happens when an infection travels deeper into the lungs, causing the tiny air sacs (the alveoli) to fill with fluid. The inflammation from bronchitis can occasionally make your lungs more vulnerable to this kind of secondary infection.
The risk is higher for certain groups:
- Older adults (over age 65)
- Infants and very young children
- Anyone with a weakened immune system
- People with existing lung conditions like COPD or asthma
Keep an eye out for warning signs like a new high fever, sharp chest pain that gets worse when you breathe deeply, or feeling seriously short of breath. If you experience any of these, you need to seek medical care right away to rule out pneumonia.
What Makes a Bronchitis Cough So Different?
A bronchitis cough definitely has its own unique personality. Unlike a simple tickle from a common cold, this cough often feels like it’s coming from deep down in your chest. It usually starts out dry and hacking before becoming "productive"—which is just a medical way of saying you're coughing up mucus. That mucus can be clear, white, yellow, or even greenish.
The biggest giveaway, though, is how long it hangs around. A cough from a cold usually clears up within a week or two. The infamous bronchitis cough is known for overstaying its welcome, often lasting for three weeks or more, long after every other symptom is gone.
If you're tired of guessing and want clear answers about your cough, ChatWithDr can help. Get a diagnosis, a personalized treatment plan, and a prescription if needed from a board-certified doctor in minutes, all from your phone. Start your consultation for just $39.99.