Picture this: you live miles from the closest doctor, and even the local clinic is struggling to keep its doors open.For millions of Americans, getting consistent, quality medical care in rural areas is a daily battle, defined by long drives and a shrinking number of healthcare options.
The Critical State of Rural American Healthcare
For the 61 million people who call rural America home, healthcare isn’t as simple as booking an appointment. It’s a complicated mess of distance, availability, and cost. This isn't just some minor inconvenience; it's a massive gap in our nation's healthcare system, where your zip code can literally determine whether you get basic medical care.
And that gap is getting wider. Fast. Imagine your nearest hospital is over 30 miles away, and you hear it might be the next one to shut down. This is the reality for almost 20% of Americans. Recent data paints a grim picture: 46% of rural hospitals are operating in the red. This financial pressure forced nearly 120 rural hospitals to close for good between 2010 and 2020, ripping critical emergency services out of communities. You can dig into the full state of rural health in this detailed report from Chartis.com.
The Human Cost of a Shrinking System
When a local clinic or hospital closes, the shockwave is felt everywhere. It’s not just an empty building; it’s a loss of doctors, nurses, and the simple peace of mind that comes from knowing help is close by. For too many, this means putting off care for chronic conditions, ignoring warning signs, or treating the emergency room as their only doctor's office.
The consequences are real and measurable, creating a domino effect of poor health outcomes:
- Delayed Diagnoses: Longer drives for screenings mean conditions like cancer or diabetes are often caught at later, more dangerous stages.
- Worse Chronic Disease Management: Trying to manage heart disease or COPD is incredibly difficult without regular check-ins with a primary care doctor.
- Increased Strain on Families: The burden falls on family members to take off work and drive loved ones to appointments hours away, adding a huge financial and emotional toll.
This reality turns a routine health issue into a logistical nightmare. A simple check-up can become an all-day ordeal involving hours on the road, lost wages, and steep gas prices.
A Population in Greater Need
On top of all this, rural America is aging faster than urban areas. These communities have a higher percentage of older adults who naturally have more complex health needs and chronic illnesses. This puts even more strain on a healthcare system that's already stretched to its absolute limit.
The need for dependable medical care in rural areas has never been more critical. As traditional hospitals and clinics fight to survive, the search for practical, accessible solutions isn't just about convenience—it's a matter of life and death. Every time a facility closes, it creates a healthcare desert, forcing residents to ask a terrifying question: "Where do we go when we get sick?" This guide will explore the new answers that are starting to fill that void.
Understanding the Barriers to Care
Getting quality medical care when you live in a rural area can feel like trying to navigate a landscape full of roadblocks. It’s not just one single problem, but a tangled web of challenges that create huge hurdles for millions of Americans. These barriers aren't just inconvenient; they systematically get in the way of timely, effective healthcare, and that leads to poorer health outcomes down the line.
Imagine trying to get to a destination, but every path is blocked. First, you realize the sheer distance you have to travel is a massive obstacle. Then you find out the expert you need isn't even available in your area. Next, you discover the road itself is crumbling from a lack of funding, and to top it off, your digital map has no signal. This is a pretty good picture of what rural residents are up against.
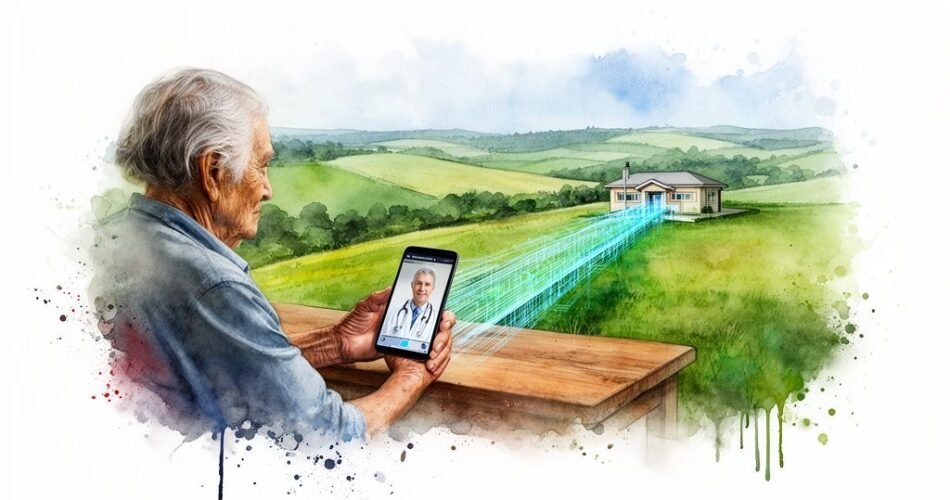
This flowchart really drives home the direct line between population dynamics and the fragile state of rural hospitals.
It shows how a population with higher needs, combined with intense financial strain, puts hospitals at risk of closing their doors for good—widening the healthcare gap even further.
To really get a handle on the situation, we need to look at the core obstacles one by one. I've broken them down into a table to make it clear.
Core Obstacles in Rural Healthcare
This table summarizes the primary challenges rural populations face in accessing consistent and quality medical care.
| Barrier Category | Description | Impact on Patients |
|---|---|---|
| Geographic Isolation | Long travel distances to clinics and specialists. | Skipped preventative care, delayed treatment for chronic conditions, high out-of-pocket costs for travel. |
| Workforce Shortages | A critical lack of physicians, specialists, and support staff. | Long wait times for appointments, limited access to specialized care, overworked and burnt-out local doctors. |
| Financial Instability | Hospitals operate on razor-thin margins due to lower reimbursement rates and a smaller patient base. | Hospital closures, reduced services, lack of investment in modern equipment and facilities. |
| The Digital Divide | Unreliable or non-existent high-speed internet access. | Inability to use telehealth services, difficulty accessing digital health records or online medical information. |
Each of these barriers feeds into the others, creating a cycle that's tough to break. But understanding them is the first step toward finding real solutions.
Geographic Isolation and Distance
The most fundamental barrier is geography itself. When the nearest clinic is a 45-minute drive and a specialist is hours away, "seeing a doctor" turns into a major logistical headache. It’s not just the time on the road; it means taking a whole day off work, figuring out childcare, and paying for gas, all for a 15-minute consultation.
This distance has a chilling effect on preventative care. Routine screenings, check-ups for chronic diseases, and important follow-up appointments often get pushed aside or skipped entirely because the effort and cost are just too high. This is how manageable conditions can quietly escalate into serious health crises.
Physician and Staffing Shortages
Even if you can make the long drive, there’s no guarantee a doctor will be there to see you. Rural America is grappling with a severe and ongoing shortage of healthcare professionals—from general practitioners to surgeons and mental health providers. Doctors are often drawn to cities by higher salaries, more opportunities, and better resources, leaving small towns in the lurch.
This scarcity creates a domino effect. The few doctors who do work in rural areas are often overworked, which leads to burnout and early retirement, making the shortage even worse. Without enough staff, clinics can't offer a full range of services, forcing patients to travel even farther for the care they need.
Financial Instability of Rural Hospitals
The financial health of rural clinics and hospitals is often incredibly fragile. These facilities typically serve populations that are older, have lower incomes, and are more likely to be covered by Medicare or Medicaid, which pay out less than private insurance. This creates a tough financial environment where many hospitals are barely breaking even or are operating at a loss.
Right now, over 700 rural hospitals across the country are at risk of closing. When a local hospital shuts down, it’s a devastating blow to the community. It wipes out the main source of emergency care and gets rid of stable, well-paying jobs, creating a void that's almost impossible to fill.
The Digital Divide
In an age where technology is supposed to be bridging gaps, the digital divide creates yet another massive barrier. While telehealth seems like a perfect solution, it only works if you have a reliable internet connection—something many rural households simply don't have. Only about 60% of rural homes have consistent broadband, which makes video consultations impossible for a huge chunk of the population.
This digital gap prevents people in rural areas from taking full advantage of modern healthcare. To really move the needle, it's critical to implement systems that are built for these specific challenges, like adopting the right EHR adoption strategies for rural and underserved healthcare facilities. If we don't address these foundational issues of access, staffing, finance, and technology, the healthcare gap in rural America will only keep getting wider.
How Telehealth Is a Lifeline for Rural Patients
When the road to the nearest clinic is long and the local hospital is struggling, technology can build a bridge. Telehealth isn't some futuristic idea; it's a practical, immediate lifeline that directly addresses the biggest barriers to getting medical care in rural areas. It acts as a digital connection, linking patients in isolated communities with board-certified doctors, bypassing the miles and the wait times.
This connection tears down the walls of distance and doctor shortages. Instead of a day-long journey for a 15-minute appointment, patients can get a diagnosis and treatment plan right from their own homes. Services like ChatWithDr are built to make this connection as simple and accessible as possible.
Rethinking the Doctor Visit
Most people hear "telehealth" and immediately think of a video call, which can be a huge problem where high-speed internet is spotty. The good news is that modern platforms offer different, more accessible ways to get care that are perfectly suited for the realities of rural life.
One of the most effective methods is asynchronous telehealth, also known as "store-and-forward" care. The easiest way to think of it is like a secure, detailed text message conversation with your doctor.
- You Start the Conversation: You kick things off by filling out a secure online form, detailing your symptoms and medical history at your own pace. No rush.
- The Doctor Responds: A licensed physician reviews your information, makes a diagnosis, and puts together a personalized treatment plan for you.
- Care is Delivered: The doctor sends you the plan, answers any questions you have, and can send a prescription to your local pharmacy if you need one—all without ever needing a live video connection.
This text-based model is a game-changer for rural patients. It only needs a basic internet or cellular connection, offering a level of privacy and convenience a video call just can't match. You can start a consultation during a lunch break or late at night, fitting healthcare into your life instead of the other way around.
From Problem to Immediate Solution
Let’s connect this back to the real-world headaches rural patients face. The traditional system forces you to wait for an appointment, drive for hours, and then sit in a waiting room. Telehealth completely flips that script, offering direct solutions.
By providing instant access to consultations and e-prescriptions, telehealth directly counters the core barriers of geographic isolation and workforce shortages. It delivers care where it’s needed most—right at home.
For instance, waking up with a painful UTI no longer means a frantic search for an open appointment and a long drive. With a service like ChatWithDr, you can describe your symptoms on a secure form and have a prescription waiting at your local pharmacy in just a few hours. That kind of speed and efficiency is vital when timely medical care in rural areas is so hard to come by. To see how these services work in detail, you can learn more about specific telehealth services and the conditions they cover.
As telehealth becomes a core part of healthcare, opportunities for professionals in telehealth jobs are also growing, which further expands access to care. This growth helps build a more robust digital healthcare workforce, ensuring more doctors are available to serve patients regardless of their zip code. This expanding network of online physicians provides the backbone for a system that can finally start to close the rural healthcare gap, one virtual consultation at a time.
Get Same-Day Care With ChatWithDr
When you’re feeling awful, the last thing you want is a logistical nightmare. This is where telehealth platforms like ChatWithDr stop being just an idea and become a real, same-day solution for getting medical care in rural areas. Instead of blowing up your whole day for a clinic visit, you can get a diagnosis and a treatment plan from a board-certified doctor right on your phone.
The whole process is designed to be simple and quick. It gets you from feeling sick to having a solution in hand, often in just a couple of hours. Let’s walk through exactly how it works, step by step.
Step 1: Start Your Secure Consultation
First things first, you’ll head over to the ChatWithDr website and pick the health issue you're dealing with. The platform is built to handle a ton of common problems that rural patients face—things like UTIs, sinus infections, pink eye, and even routine medication refills for birth control or blood pressure meds.
Once you select your condition, you'll start the secure online intake form. This isn't your average contact form; it's a detailed, HIPAA-compliant questionnaire that physicians designed to get all the critical info about your symptoms and medical history. Think of it as the conversation you’d have with a nurse before the doctor walks in, except you can do it from your couch.
Step 2: Provide Your Information
This is where you’ll lay out what’s going on. The questions are specific and guide you through providing the exact details a doctor needs to make an accurate diagnosis. You can even upload photos if they help tell the story, which is a game-changer for skin conditions like rashes or acne.
This text-based approach is a massive plus for anyone with spotty internet. You don’t need a rock-solid connection for a video call. As long as you can load a webpage, you're good to go. At the end, you’ll pay the flat $39.99 consultation fee. No surprises.
Step 3: Get Your Diagnosis and Treatment Plan
After you hit submit, a board-certified, state-licensed U.S. physician gets to work reviewing your case. They'll carefully go over your symptoms and medical history to figure out what's wrong and create a personalized treatment plan just for you.
You'll get this plan sent directly to you through the secure platform. It will clearly explain your diagnosis, give you treatment instructions, and answer any questions you might have. The whole process is incredibly efficient—many patients have their plan in hand in just 1-2 hours.
By taking travel and appointments out of the equation, this model turns healthcare from a location-based service into an on-demand resource. It puts expert medical care directly into the hands of people who need it most, no matter their zip code.
Step 4: Receive Your Prescription Locally
If your treatment plan includes a prescription, the doctor will send it electronically to whatever pharmacy you choose. This feature is absolutely crucial for delivering effective medical care in rural areas. You can pick your small, local pharmacy—you’re not forced to use a big chain.
The e-prescription is sent immediately, so you can often pick up your medication the very same day. This last step closes the loop on your care, making sure you not only get a diagnosis but also have the medicine you need to start feeling better right away. The platform’s ability to handle common urgent care needs makes it a powerful tool for getting immediate relief. You can learn more about how they handle non-emergency issues by reading about their online urgent care services.
Of course. Here is the rewritten section, crafted to sound like an experienced human expert and match the provided examples.
Figuring Out the Cost and Legitimacy of Telehealth
When you're dealing with a health issue, the last thing you want to worry about is a confusing bill or whether the doctor you're talking to is even legitimate. For telehealth to really make a difference in rural medical care, it has to be built on trust. That means tackling the practical stuff head-on, from what it costs to who is providing the care.
A big first step is understanding how you'll pay. Many telehealth services, like ChatWithDr, have moved to a simple flat-fee model. You pay one price for the whole consultation—no hidden fees, no surprise bills in the mail later. For families on a tight budget, knowing the exact cost upfront is a massive relief.
This kind of straightforward pricing takes away the financial stress that so often comes with healthcare, making it easier to just get the help you need, when you need it.
Navigating Payment and Insurance
A common question is how telehealth works with different payment methods and insurance. The flexibility here is a huge plus for patients who need options.
Most modern platforms are built to make payment as painless as possible:
- HSA/FSA Cards: You can almost always use your Health Savings Account (HSA) or Flexible Spending Account (FSA) card. This lets you pay with pre-tax dollars, stretching your healthcare budget even further.
- Direct Payment: Of course, standard credit and debit cards are always an option, making the service accessible to pretty much anyone.
It's also important to get how insurance fits into the picture. While you pay the platform directly for the consultation, your health insurance comes into play where it really counts—at the pharmacy. If the doctor prescribes medication, you can use your insurance to cover it, just like you would after an in-person visit.
This hybrid approach really gives you the best of both worlds: a clear, low-cost fee for the doctor's time and the ability to use your insurance benefits to keep prescription costs down.
Ensuring Your Care is Safe and Legitimate
Beyond the cost, the biggest question for most people is whether an online doctor service is actually safe. The answer comes down to two non-negotiable standards that any reputable platform has to meet: HIPAA compliance and state-licensed physicians. These aren't just buzzwords; they're strict legal shields that protect you and guarantee quality care.
HIPAA (Health Insurance Portability and Accountability Act) is the federal law that sets the gold standard for protecting your sensitive health information. A HIPAA-compliant platform uses heavy-duty security to make sure your personal details and medical history stay completely private.
On top of that, every single doctor you see on a legitimate platform must be a board-certified physician licensed to practice medicine in your specific state. This is a deal-breaker. It ensures the person diagnosing you has met the tough educational and professional hurdles required to provide care where you live. This verification means you're not just talking to a doctor; you're talking to a qualified professional legally authorized to treat patients in your community.
Knowing When to Use Telehealth vs. In-Person Care
Telehealth is an incredibly powerful tool, especially for improving medical care in rural areas, but it’s not meant to replace every single trip to the doctor. The real key to using it safely and effectively is knowing its strengths and, just as importantly, its limits.
Think of it like having a well-stocked first-aid kit at home. It’s perfect for handling urgent but non-critical problems on the spot. But you’d still call 911 for a true, life-threatening emergency, right?
Making that distinction helps you get the right level of care exactly when you need it. It’s all about empowering you to make smart, safe decisions for your health.
When Telehealth Is Your Best Option
Telehealth really shines when you're dealing with common, low-risk conditions that a doctor can diagnose based on your symptoms and medical history. It's the ideal choice when you need a quick, convenient answer without a hands-on physical exam.
Consider using a telehealth service for issues like:
- Common Infections: Things like UTIs, sinus infections, pink eye, and bronchitis can often be diagnosed and treated just by describing your symptoms in detail.
- Skin Conditions: For rashes, acne, or other minor skin irritations, snapping a clear photo can give a doctor all the visual information they need to help.
- Medication Refills: If you need a refill for a stable, ongoing prescription—like birth control or blood pressure medicine—telehealth is a fast, straightforward solution.
- Minor Ailments: Problems like migraines, allergies, or a bout of nausea are perfectly suited for a virtual chat with a doctor.
The core idea is simple: if your condition can be safely figured out through a good conversation and maybe a photo, telehealth is probably a fantastic fit. It’s built for speed and access for non-emergency care.
When You Absolutely Need In-Person Care
On the flip side, some situations are non-negotiable and demand immediate, in-person medical attention. Telehealth cannot—and should not—try to replace emergency services or a hands-on examination. Always dial 911 or get to the nearest emergency room for any life-threatening symptoms.
Situations that require in-person care include:
- Emergencies: Chest pain, trouble breathing, severe bleeding, sudden weakness or numbness on one side of your body, or major injuries are all red flags. These require immediate emergency services.
- Hands-On Exams: If you're dealing with severe abdominal pain, think you might have a broken bone, or need stitches, a doctor has to physically examine you.
- Complex Chronic Conditions: Managing complicated, long-term health issues often requires ongoing physical check-ins and tests that can only be done at a clinic.
Knowing the difference is vital. Our guide to online primary care can help you learn more about the kinds of ongoing health needs that can be managed virtually.
Got Questions About Rural Telehealth?
Jumping into telehealth for the first time can feel a little strange, so it's natural to have questions. Let's clear up some of the most common concerns so you can feel confident getting top-notch medical care in rural areas right from your phone.
Is an Online Doctor Service Legitimate and Safe?
Yes, absolutely. A reputable service like ChatWithDr is a HIPAA-compliant platform, meaning your private health information is guarded by the same strict federal laws that protect you in a physical doctor's office.
Every single physician on the platform is board-certified and licensed to practice in your specific state. This isn't just a promise; it's a legal requirement. It ensures they meet all the standards for making diagnoses, creating treatment plans, and sending prescriptions. With a history of helping over 50,000 patients and a 4.9-star rating, you know you're in good hands.
What If I Have Bad Internet for a Video Call?
This is where a text-based platform really shines. We know that spotty broadband is a huge headache in rural areas, so the entire consultation is designed to work without video. You never need a strong, stable internet connection.
You simply fill out a secure online form with your symptoms when you have a signal. The whole process is asynchronous, which means you and the doctor communicate without needing to be online at the same exact time. This design choice removes one of the biggest roadblocks to getting care when you live miles from anywhere.
How Can a Doctor Diagnose Me Without an In-Person Exam?
You’d be surprised how much an experienced doctor can diagnose without a physical exam. For many common urgent care issues—think sinus infections, UTIs, or pink eye—a detailed description of your symptoms and your medical history is more than enough for an accurate diagnosis.
Our secure intake form is carefully designed by physicians to gather all the critical information needed to safely evaluate your condition. It’s the same structured conversation you'd have in a clinic, just more efficient.
For things like skin rashes, you can even upload a photo, which is often clearer than what a doctor can see in a poorly lit exam room.
Can I Get a Prescription Sent to My Local Pharmacy?
Of course. If your treatment plan includes a prescription, our doctors send it electronically to any pharmacy you choose in the United States. This includes the small, independent pharmacies that are the heart of many rural towns.
During your intake, you'll just provide your preferred pharmacy’s information. The e-prescription is sent there directly, so you can pick it up—often within just a few hours of your consultation.
Ready to skip the drive and the waiting room? ChatWithDr offers same-day treatment from board-certified doctors for just $39.99. Get the care you need, right where you are. Start your secure consultation now.